| Azooka Labs unveils Safe MTM to Store COVID-19 Samples at Room Temperature for up to a week Molecular Transport Medium at the price of VTM BANGALORE, India – December 15th, 2020 Azooka Labs, a leading safe fluorophore company with specialization in Molecular Biology products, reveals its first range of novel COVID-19 diagnostics products. RNA Wrapr is a molecular transport medium for COVID-19 sample collection, developed as part of the COVID-19 response team from Indian Institute of Science. RNA Wrapr inactivates the virus immediately only preserving DNA/RNA content required for RT-PCR tests. The sample tubes can be stored up to 7 days in Room Temperature and transported without dry ice or gel packs. RNA Wrapr is safe to handle even during unexpected accidental spillage or handling errors. Developing countries can collect samples in centers without BSL2 or BSL3 certifications. Azooka's RNA Wrapr is priced at INR 99* in India, aligned with the price of one litre of petrol, to help the diagnostic centers upgrade from VTM to MTM. Azooka plans to enter the APAC market through partners with $9 and $6 pricing plans per test. "Azooka has actively been a part of the fight against COVID by developing PCR and RT PCR kits with support from Dept of Biotechnology and Elevate Karnataka even before the pandemic hit us" quoted Alex D Paul, CEO, Azooka Labs. He further added, "MTM has ensured safety and security of COVID-19 samples to be stored at Room Temperature for up to seven days". "Azooka is the only startup from India working to replace Carcinogenic and Mutagenic SYBR dyes widely used in RUO and Diagnostics reagents. Safety and cost savings needed for COVID crisis management today are the highlights of Azooka's MTM" says Dr. C V Natraj, former SVP, Corporate Research, Unilever plc. "Azooka is striving to provide a safer molecular grade transport medium that is at sub Rs. 100. We are appealing to a segment of users, who care about the safety of their frontline health care workers", stated Dr. Fatima Benazir, Co-founder & CSO, Azooka Labs. About Azooka Labs:Azooka is a patented fluorophore company focused on developing safe biotech consumables at a price affordable for all countries across the globe. Azooka's first diagnostics product RNA Wrapr- molecular transport medium, is approved by ICMR and certified by CE. Azooka is an IISc invested startup based in Bengaluru with R&D unit at the Indian Institute of Science and manufacturing facility in Peenya Industrial Area, Karnataka. Azooka was recently awarded the 'Best Women-Led Enterprise' at StartUp India 2020. Azooka is open for licensing and partnerships worldwide. Governments and Health Organizations can directly contact Azooka for COVID-19 Crisis Management. For more information visit: http://azooka.life/ and for the prices visit: https://azooka.life/rna-wrapr-molecular-transport-medium/ |
Author: trainitright
New Study Gives Canada a "B" Grade for Overall Cancer Mortality
Improvements in screening, early detection, and treatment contribute to decreased risk of dying from cancer in Canada
Canada's mortality rate due to lung cancer is high compared to most peer countries
Differences exist in overall cancer mortality rates among the provinces
MISSISSAUGA, ON, Dec. 15, 2020 /CNW/ - According to Mortality Due to Cancer 2020: Benchmarking Cancer Mortality in Canada, a new study examining the performance of Canada and its provinces on a number of health indicators, including mortality due to cancer, Canada earns a "B" mark when it comes to overall mortality due to cancer. Gaps in performance across the provinces suggest room for improved management of the disease.

The study, conducted by Conference Board of Canada and commissioned by Amgen Canada, compared the age-standardized mortality rates (ASMR) of Canada and the provinces against 16 peer countries with similar economic and socio-demographic profiles.1
While the report examined the combined mortality of over 100 types of cancer, the report focused on mortality rates for three common types: lung, colorectal, and prostate.2 These three cancer types combined account for over 40 per cent of mortality due to cancer.
Overall, the study found the following:
- Canada ranks average for the overall cancer mortality rate, and for the mortality rate due to prostate cancer and colorectal cancer.
- Canada's mortality rate due to lung cancer is high compared to most peer countries.
- British Columbia, Ontario, and Alberta consistently perform better than other provinces.
- The Atlantic provinces have higher cancer mortality rates than the rest of the country.
- Canada needs a diverse approach to improving oncology outcomes that includes prevention, early detection, and better access to treatments.
Study Results
According to Mortality Due to Cancer 2020, for all cancers combined,3 Canada ranks in the middle —placing eighth out of 17 comparator countries — with 190 deaths per 100,000 population.
While Canada scores a "B," the performance of the provinces compared to the 17 countries varies widely. British Columbia is the only province that scores an "A" grade compared to other countries, followed by Alberta and Ontario, with each receiving a "B" grade. Newfoundland and Labrador and Nova Scotia have the highest mortality rates of 222 and 216 deaths per 100,000 population, respectively.
Policy implications and conclusions
"Canada's "B" grade for overall mortality rate due to cancer and for prostate and colorectal cancers specifically means that while Canada performs better than half of comparator countries, there is much room for improvement," says Dr. Monika Slovinec D'Angelo, Director, Health, The Conference Board of Canada.
Unfortunately, long waits to access cancer drugs, challenges related to public and private insurance plans, the lengthy approval process for new oncology drugs, and the lack of critical population mass required to offer innovative or costly treatments in some provinces are among the reasons access to innovative oncology treatments lags in Canada.
According to the study, a multi-pronged approach is essential to improve oncology outcomes. "Our research underscores the important role prevention, early detection and screening, and better access to innovative diagnostics and treatments play in improving the management of cancer in Canada," says Dr. Slovinec.
About Mortality Due to Cancer 2020: Benchmarking Cancer Mortality in Canada
A report-card style ranking was used to assess the performance of Canada and the provinces.
For the purposes of this report, Canada was benchmarked against 16 comparator countries including Australia, Austria, Belgium, Denmark, Finland, France, Germany, Ireland, Italy, Japan, the Netherlands, Norway, Sweden, Switzerland, the United Kingdom, and the United States of America.
For each type of cancer, jurisdictions received a rating based on the distance and relationship of its in age-standardized mortality rate (ASMR) to the mean of the ASMRs.
"We are pleased to support this analysis of cancer mortality in Canada," says Dr. Suna Avcil, Executive Medical Director at Amgen Canada. "While much progress has been made in the diagnosis and treatment of this disease, Amgen remains committed to helping identify areas of high unmet medical need and looking for solutions that improve health outcomes and dramatically improve people's lives."
About Cancer in Canada
Cancer accounts for nearly one-third of deaths in Canada.4 In 2020, an estimated 225,800 Canadians will be diagnosed with cancer, with 83,300 deaths resulting from the disease.5 Lung, breast, colorectal, and prostate cancers will account for nearly half of new cancer cases in Canada in 2020.6
The annual number of new documented cancer cases is increasing in Canada. However, this increase is driven by demographic growth and aging as well as improved detection and screening, not by an increased prevalence of cancer.
Despite the increased incidence, there has been a steady decrease in age-standardized mortality rate (ASMR) since 2003; this indicates that the risk of dying from cancer is being reduced in Canada. This decline has been attributed to improvements in screening, early detection, and treatment.7
While deaths from cancer in Canada have decreased over the past two decades, but many are still avoidable.
About The Conference Board of Canada
The Conference Board of Canada is the country's leading independent research organization. Our mission is to empower and inspire leaders to build a stronger future for all Canadians through our trusted research and unparalleled connections. Follow The Conference Board of Canada on Twitter @ConfBoardofCda
About Amgen Canada
As a leader in innovation, Amgen Canada understands the value of science. With main operations located in Mississauga, Ontario's vibrant biomedical cluster, and its research facility in Burnaby, B.C., Amgen Canada has been an important contributor to advancements in science and innovation in Canada since 1991. The company contributes to the development of new therapies and new uses for existing medicines in partnership with many of Canada's leading health-care, academic, research, government and patient organizations. To learn more about Amgen Canada, visit www.amgen.ca.
| ___________________________________ |
| 1 Peer countries to Canada include Australia, Austria, Belgium, Denmark, Finland, France, Germany, Ireland, Italy, Japan, the Netherlands, Norway, Sweden, Switzerland, the United Kingdom, and the United States of America |
| 2 Cancer types are defined using the ICD-10 classification, a medical classification list developed and updated by the World Health Organization. Lung cancer refers to malignant neoplasms of the trachea, bronchus, and lung. Colorectal cancer refers to malignant neoplasms of the colon, rectum, anus, and anal canal. Prostate cancer refers to malignant neoplasm of the prostate |
| 3 Includes malignant neoplasms of breast, lung, colorectal, prostate, pancreas, liver, lymphoid, and hematopoietic, along with other less prevalent tumour sites (over 100 types of cancer in total) |
| 4 Canadian Cancer Society, "Cancer Statistics at a Glance." |
| 5 Brenner and others, "Projected Estimates of Cancer in Canada in 2020." |
| 6 Excludes non-melanoma skin cancer |
| 7 Canadian Cancer Statistics Advisory Committee, Canadian Cancer Statistics 2018 |

SOURCE Amgen Canada
Online Health Promotion Program Shown to Significantly Improve the Physical and Mental Health of Canadians During the Pandemic
MONTREAL, Dec. 15, 2020 /CNW/ - During the Covid 19 pandemic, over 100 Canadians joined the MissionVAV Drop 5 Mission to: increase their daily physical activity, improve their healthy food choices, reduce their fatigue and stress levels, drop unwanted pounds, and improve their sleep. The web-based health program, developed by researchers and health professionals at the McGill Comprehensive Health Improvement Program (CHIP), came to an end on November 29. Preliminary results are now available and final results will be presented at medical research meetings in 2021.

Over 75% of participants completed the 10-week program. Each week where they were trained to adopt a new healthy lifestyle habit, track their progress, and receive regular feedback and health coaching from volunteer medical students studying at McGill University. The following results were observed:
- 88% completed 30 or more minutes of regular physical activity at least 5 days per week
- 76% reduced their stress levels by at least 5%
- 62% reduced their fatigue by at least 5%
- 56% improved their sleep quality by at least 5%
- 39% reduced their weight by at least 5 pounds.
Dr Steven Grover, a Professor of Medicine at McGill University, and one of the co-leaders of this program noted: "The high completion rate is extraordinary and probably reflects the substantial impact of the excellent health coaching provided weekly by the medical students. Not only did this help to keep participants engaged but it undoubtedly played an essential role in some of the more challenging lifestyle changes such as losing excess body weight. Feedback from the students was also very positive as they learned first-hand about the challenges of motivating their future patients to adopt healthy habits".
The next Drop 5 Mission will start January 11, 2021 and will again run for 10 weeks (funded by Veterans Affairs Canada). It is fun and free, not only for Canadian Veterans and their families, but also for other Canadian's who are trying to maintain or improve their health during the pandemic.
SOURCE McGill Comprehensive Health Improvement Program (CHIP)
For further information:
Dr Steven Grover, steven.grover@mcgill.ca, 514-791-5688
Health Canada Approves VENCLEXTA® (venetoclax) in combination with azacitidine or low dose cytarabine for untreated Acute Myeloid Leukemia (AML)
- Health Canada's approval of VENCLEXTA for newly diagnosed AML patients who are ineligible for intensive chemotherapy is supported by data from two Phase 3 trials - VIALE-A (M15-656) and VIALE-C (M16-043)1.
- The VIALE-A trial demonstrated a statistically significant increase in overall survival with VENCLEXTA in combination with azacitidine compared to azacitidine alone.1
- In the VIALE-C trial, clinical benefit was based on rate and duration of complete response.1
- AML is one of the most difficult-to-treat blood cancers with a very low survival rate.2,3
MONTREAL, Dec. 15, 2020 /CNW/ - AbbVie (NYSE: ABBV), a research-based global biopharmaceutical company, announced today that Health Canada has approved VENCLEXTA® (venetoclax) in combination with azacitidine or low-dose cytarabine (LDAC) for the treatment of newly-diagnosed acute myeloid leukemia (AML) in adults who are age 75 years or older, or who have comorbidities that preclude the use of intensive induction chemotherapy. AML is an aggressive and difficult-to-treat blood cancer with a low survival rate.2,3 In Canada, the five-year survival rate for patients diagnosed with AML is approximately 21%.3
"AML is one of the most common types of leukemia in adults. AML progresses rapidly and has a significantly lower survival rate compared to other cancers. Having more effective treatment options for AML patients will improve treatment outcomes for Canadians and extend lives," said Dr. Brian Leber, Head of Leukemia Service at the Juravinski Hospital and Cancer Centre.
In the VIALE-A trial, the median overall survival of patients who received VENCLEXTA plus azacitidine was 14.7 months (11.9, 18.7) vs 9.6 months (7.4, 12.7) in patients who received azacitidine in combination with placebo. In the VENCLEXTA plus azacitidine arm, the most frequent serious adverse reactions (≥ 5%) were febrile neutropenia (30%), pneumonia (23%), sepsis (16 %) and hemorrhage (9%)1.
"With limited treatment options, it makes me very happy to know that VENCLEXTA has been approved to treat others, like me, who are diagnosed with AML," said William Levine of Courtice, Ontario.
In the VIALE-C trial, clinical benefit was based on the rate of complete responses (CR) and duration of CR, with supportive evidence of the rate of CR + CRi (complete remission with incomplete blood count recovery), duration of CR + CRi and the rate of conversion from transfusion dependence to transfusion independence. 27 % of patients achieved CR in the VENCLEXTA plus LDAC arm vs 7% of patients treated with Placebo+ LDAC. In the VENCLEXTA + LDAC arm, most frequent serious adverse (≥ 5%) were pneumonia (18%), febrile neutropenia (16%), sepsis (11%), hemorrhage (9%), and thrombocytopenia (5%)1.
"Every day, we aim to transform the standard of care for people living with cancer," said Denis Hello, Vice President and General Manager, AbbVie Canada. "Having effective and proven treatment options is vital for patients and their families impacted by AML."
Health Canada's approval was granted under Project Orbis, an FDA initiative which provides a framework for concurrent submission and review of oncology products among international partners.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the U.S. and by AbbVie outside of the U.S.
About AbbVie in Oncology
At AbbVie, we strive to discover and develop medicines that deliver transformational improvements in cancer treatment by uniquely combining our deep knowledge in core areas of biology with cutting-edge technologies, and by working together with our partners – scientists, clinical experts, industry peers, advocates, and patients. We remain focused on delivering these transformative advances in treatment across some of the most debilitating and widespread cancers. We are also committed to exploring solutions to help patients obtain access to our cancer medicines. AbbVie's oncology portfolio consists of marketed medicines and a robust pipeline containing multiple new molecules being evaluated worldwide in more than 300 clinical trials and more than 20 different tumor types.
About AbbVie
AbbVie's mission is to discover and deliver innovative medicines that solve serious health issues today and address the medical challenges of tomorrow. We strive to have a remarkable impact on people's lives across several key therapeutic areas: immunology, oncology, neuroscience, eye care, virology, women's health and gastroenterology, in addition to products and services across its Allergan Aesthetics portfolio. For more information about AbbVie, please visit us at www.abbvie.ca and www.abbvie.com. Follow @abbvieCanada and @abbvie on Twitter or view careers on our Facebook or LinkedIn page.
___________________________
1 AbbVie Corporation Venclexta(R) (venetoclax) Product Monograph. Date of Preparation: September 27, 2016. Date of Revision: December 3, 2020.
2 Leukemia & Lymphoma Society of Canada. Acute myeloid leukemia (AML). https://www.llscanada.org/leukemia/acute-myeloid-leukemia. Accessed November 25, 2020.
3 Canadian Cancer Society. Survival statistics for acute myelogenous leukemia. https://www.cancer.ca/en/cancer-information/cancer-type/leukemia-acute-myelogenous-aml/prognosis-and-survival/survival-statistics/?region=on Accessed November 25, 2020.
SOURCE AbbVie
CORDANT HEALTH SOLUTIONS AND SPERO HEALTH INCREASE NALOXONE ACCESS, SAVE LIVES
PIKEVILLE, Ky., Dec. 15, 2020 -- Cordant Health Solutions®, a leader in providing innovative tools for patients in addiction treatment programs, and Spero Health, an integrated health services organization specializing in the treatment of patients with opioid use disorder, today announced promising results in a new initiative to increase patient awareness of access to naloxone.
Over the last eight months, Cordant has worked with Spero to provide convenient access to medication-assisted treatment (MAT) prescriptions across clinics in Kentucky and Tennessee, including prescriptions for the lifesaving overdose-reversal drug naloxone.
Rising regional fentanyl use has alarmed addiction specialists, including Dr. Byron Crider, a provider at Spero’s largest clinic in Kentucky. "The Pikeville area saw four overdose deaths in four days. Now more than ever is the time to educate patients and get naloxone to them in a proactive way to help keep them safe," he said.
At Spero Health, clinicians have candid and open conversations with patients about recovery and risk prevention. The patients then receive delivery of their prescribed naloxone while still at the clinic through Cordant’s managed pharmacy program. During the summer, 486 of Cordant’s MAT pharmacy patients at two of Spero’s treatment clinics in eastern Kentucky received naloxone at their addiction treatment appointment.
"Four of my patients have already used their initial prescription on a friend or loved one, so I regularly check to see who needs refills," said Crider. "Just as we keep a fire extinguisher in our homes should the unthinkable occur, MAT patients should carry naloxone to protect themselves and their loved ones. Many of my patients have told me they would have never thought about having naloxone in their home, but they are thankful they did."
"Many providers don’t focus on naloxone as part of addiction treatment, yet research shows that access to naloxone decreases overdose deaths," said Daniel Mandoli, Cordant’s president of pharmacy services. "Delivering naloxone to patients at their office visit through our onsite program ensures they receive it, which is an important step in the process."
In 2018, almost 47,000 people died of an opioid overdose, and preliminar data from 2019 and 2020 shows this pattern continuing to climb. The U.S. Office of the Surgeon General stated that over 50% of opioid overdose deaths occur in the home and has urged for greater access to naloxone to prevent further deaths.
####
If you have any questions or would like to interview Dr. Crider please let me know.
Tiffany Tuetken
Sr. Director of Marketing and Communications
ttuetken@cordanths.com
303-570-4585
About Cordant Health Solutions
Cordant Health Solutions® (cordantsolutions.com) provides innovative tools for monitoring behavioral health, chronic pain and criminal justice cases. Cordant’s unique pharmacy and drug testing programs provide accurate, actionable results to protect prescribers, hold patients accountable and optimize quality of life.
A leader in quality standards, Cordant provides solutions for payers, clinicians and organizations involved with substance use disorder, pain management and criminal justice agencies. Cordant is one of the only healthcare companies that offers monitoring and risk assessment tools through its innovative drug testing options and full-service, high-touch pharmacies, which specialize in the management and dispensing of addiction treatment medications. Cordant’s testing protocols and digital case-management tools help clients become more efficient and effective in using drug testing programs to monitor patient adherence, reduce risk and improve patient outcomes.
About Spero Health
Spero Health, (sperohealth.com) Inc., is an integrated healthcare services organization specializing in local and affordable outpatient care for individuals suffering from substance use disorders with a mission to "Save Lives, Instill Hope, and Restore Relationships." Spero Health utilizes an innovative, evidence-based integrated care model that combines both physical and behavioral healthcare services under one roof to treat the whole patient. This integrated care model combines physician services (including medication-assisted treatment), behavioral health counseling, recovery support services, medication management and patient and family education. Its community-based approach to treatment allows patients to continue working and caring for their families as they overcome addiction.
Based in Nashville, Tenn., and privately held by Heritage Group, Health Velocity Capital, South Central, Inc., and Frist Cressey Ventures, Spero Health operates over 45 outpatient clinics located throughout Kentucky, Indiana, Virginia and Tennessee. Providing care for more than 8,500 patients, Spero is one of the largest office-based opioid treatment providers in the country and is in-network with Medicaid and most commercial insurance plans.
Canadian Vaccine Catalogue releases critical standardized terminology for COVID-19 vaccines
OTTAWA, ON, Dec. 15, 2020 /CNW/ - Standardized vaccine terminology and product information will be critical in the rollout of COVID-19 vaccines to ensure consistency across Canada.
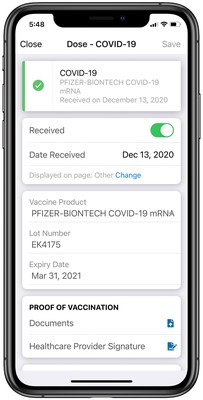
The Canadian Vaccine Catalogue (CVC) is the comprehensive, standards-based resource for vaccine terminology and vaccine product information in the country. CANImmunize, which created the CVC, has updated the resource with the latest COVID-19 vaccine codes and information.
"It is essential that digital systems tracking COVID-19 vaccinations use the standardized terminology in the Canadian Vaccine Catalogue to ensure people receive the correct vaccine for their second dose, and to help with safety and effectiveness assessments," says Cameron Bell, Chief Technology Officer, CANImmunize.
This standardized vaccine terminology is essential for governments, electronic medical record vendors and any organization tracking COVID-19 immunization data, as it will permit the timely aggregation and reporting of data across the country for surveillance purposes.
Features
- Standardized terminology and COVID-19 vaccine product information to allow real-time capture and digital exchange of immunization records across healthcare domains and jurisdictions.
- Includes vaccine DIN, lot and expiry information directly from Health Canada, Global Trade Item Numbers to support vaccine barcode scanning, and leverages the SNOMED CT Canadian Edition Immunization codes published and maintained by Canada Health Infoway.
Tradename COVID-19 vaccine codes:
- 28581000087106 – PFIZER-BIONTECH COVID-19 messenger ribonucleic acid 30 micrograms per 0.3 milliliter suspension for dilution for injection Pfizer Canada ULC-BioNTech Manufacturing GmbH (real clinical drug)
- 28571000087109 – MODERNA COVID-19 messenger ribonucleic acid-1273 100 micrograms per 0.5 milliliter liquid for injection Moderna Therapeutics Inc. (real clinical drug)
Generic COVID-19 vaccine codes:
- 28531000087107 – Vaccine product against disease caused by Severe acute respiratory syndrome coronavirus 2 (medicinal product)
- 1119349007 – Vaccine product containing only Severe acute respiratory syndrome coronavirus 2 messenger ribonucleic acid (medicinal product)
COVID-19 Antigen code:
- 840536004 – Antigen of Severe acute respiratory syndrome coronavirus 2 (substance)
COVID-19 Disease code:
- 840539006 – Disease caused by Severe acute respiratory syndrome coronavirus 2 (disorder)
British Columbia Provincial Health Services Authority and the Ontario Ministry of Health and Long-term Care currently use the CVC to configure their immunization repositories. The CVC also populates the vaccine information in the CANImmunize Clinic Flow product and the public CANImmunize app.
The catalogue is maintained and made available for national use through funding from Canada Health Infoway.
Explore the Canadian Vaccine Catalogue here.
ABOUT CANImmunize
CANImmunize is a technology company specializing in immunization software. It developed the CANImmunize platform, a pan-Canadian digital immunization tracking system that helps Canadians keep track of their vaccinations with a mobile app and web portal. The team offers digital solutions to businesses, health care organizations and governments for vaccinations and tracking, and is preparing for the COVID-19 vaccine rollout.
SOURCE CANImmunize
Switch Health Receives Health Canada Authorization for COVID-19 At-Home Collection Kits
- Health Canada authorizes Switch Health's COVID-19 at-home specimen collection kits.
- At-home specimen collection kits will soon be available online and in participating pharmacy retailers.
- Switch Health launches proprietary videoconferencing software, ASMO, for step-by-step instructional support for guided collection at-home. ASMO connects directly to partner laboratories for fast and secure results.
- The company continues to work with provinces to bring COVID-19 at-home collection kits to market.
TORONTO, Dec. 15, 2020 /CNW/ - Switch Health, a Canadian healthcare company and industry leader in testing solutions, is pleased to announce Health Canada authorization for the company's COVID-19 at-home specimen collection kits.

The collection kits will provide Canadians with accessible and reliable testing nationwide. At-home collection kits are best suited for asymptomatic individuals who require testing for work, travel or desire regular screening. The kits are enabled via Switch Health's proprietary PHIPA-compliant videoconferencing software, ASMO, where patients are provided step-by-step instructions for proper self-collection.
Switch Health's COVID-19 at-home specimen collection kits mark the first of many at-home kits that the company plans to roll out in 2021 and reinforces the company's long-term goal of at-home testing and at-home diagnostics to provide better care for Canadians.
"We want to thank Health Canada for the collaborative discussions that resulted in the company's ability to bring this innovative solution to Canada's fight against COVID-19. We look forward to continuing conversations at the provincial level to bring the at-home collection kits to market", says Dilian Stoyanov, Chief Executive Officer of Switch Health.
Switch Health's COVID-19 at-home specimen collection kits provide a Canadian made, all-in-one solution for those requiring asymptomatic testing and will be available as soon as provinces provide approval. The release of Switch Health's proprietary software, ASMO, in conjunction with at-home kits mark two significant milestones for the fast-growing healthcare company who continues to drive forward local innovation in the fight against COVID-19 and beyond.
Rapid Growth in FY 2020
Switch Health's exponential growth in FY 2020 can be attributed to the company's rapid response to creating pandemic solutions. The company now employs over 120 Canadians nationwide and expects that number to double in the next 6 months. Switch Health's local and global top-tier partnerships have contributed to the company's expansion.
While Switch Health continues to find solutions for the fight against COVID-19, the company is focusing on future research and development in artificial antibodies and preventative medicine through AI-powered at-home diagnostic hardware and software.
About Switch Health
Switch Health is a Toronto-based healthcare company dedicated to providing better care at-home for Canadians. Switch Health has quickly become an industry leader in COVID-19 testing solutions and will be rolling out additional at-home testing and at-home diagnostic hardware and software services in 2021. Switch Health currently offers mobile rapid testing and in-clinic testing services to clients across Ontario, Alberta, Nova Scotia and New Brunswick. Switch Health's travel offering provides reliable PCR testing with fast results for eight major airline partners and their passengers.
For more details on Switch Health, please visit www.switchhealth.ca
At-home specimen collection kits will be available soon in Canada, to join the waitlist please visit https://homekit.switchhealth.ca/.

SOURCE Switch Health Solutions Inc.
I get all of my shoes from The Shoe Fairy!
I started out simply buying them because I loved their look and style and then they sponsored me.
I never promote or work with brands that I don't truly believe in!
So here are some of my favs!
Use Code: Trainitright at checkout to save an extra 10%

Ontario's doctors' plans for delivering COVID vaccine more urgent in face of record 2,275 daily cases
TORONTO, Dec. 15, 2020 /CNW/ - Ontario's doctors expressed concern that a record 2,275 Ontarians have tested positive for COVID-19 in one day and call on the government to ensure that initial limited supplies of the vaccine are given to those most at risk of being exposed to the virus.

In addition to health-care workers and people who live and work in long-term care homes, the government needs to use real-time data to track geographic areas where the virus is spreading fast and give priority to their residents.
The Ontario Medical Association today released Shining a Light at the End of the Tunnel, a comprehensive set of recommendations to ensure as many people as possible get vaccinated.
Dr. Samantha Hill, president of the Ontario Medical Association, assured Ontarians that the COVID vaccines are safe and that getting vaccinated is one of the most important things they can do to protect themselves and others.
Until a large number of people are vaccinated, it's important to continue to practice good hygiene, including physical distancing, wearing a mask and frequent hand washing, Dr. Hill said.
The new OMA white paper also recommends:
- Administering vaccines in convenient locations — such as hospitals for health-care workers, schools for staff and students and mobile vans for people unable to leave their homes.
- Moving quickly to book arenas, convention centres and other large indoor and outdoor spaces with cold storage facilities and parking facilities or access to public transportation, as part of government's plans to prepare for possible mass vaccination clinics.
- Planning should begin now in anticipation of an approved vaccine for children under 16.
- Undertaking an education campaign to combat vaccine hesitancy and misinformation.
- Enabling the use of smart phones to make appointments to get the COVID vaccine and receive reminders if they need a booster shot. The smart phone system should align with each type of vaccination, advise primary care physicians when their patents get each dose and provide consent and other information and forms.
- Developing security precautions to ensure vaccines are not stolen and to shut down criminal behaviour around the falsification or illegal advertising of vaccines, including fake websites, scams and false cures.
"The arrival of the first in what are expected to be a series of different COVID vaccines is an exciting development in what we all hope will be a return to a 'new normal' in 2021," said OMA CEO Allan O'Dette. "Until vaccines are broadly available, we must continue to follow the advice or our public health doctors to protect ourselves and each other. This is how we get our economy back on track."
About the OMA
The Ontario Medical Association represents Ontario's 43,000-plus physicians, medical students and retired physicians, advocating for and supporting doctors while strengthening the leadership role of doctors in caring for patients. Our vision is to be the trusted voice in transforming Ontario's health-care system.
SOURCE Ontario Medical Association
CSACI Statement on potential adverse reactions to COVID-19 vaccines
OTTAWA, ON, Dec. 15, 2020 /CNW/ - The Canadian Society of Allergy & Clinical Immunology (CSACI) is aware of media reports of two healthcare workers at the National Health Services in the United Kingdom (UK) who experienced adverse reactions on December 8, 2020 after receiving the Pfizer/BioNTech vaccine for COVID-19. This is the same vaccine that was approved for use in Canada on December 9, 2020. Subsequent to the UK reports, Public Health England in the UK made initial broad cautionary recommendations.

The CSACI is the largest national professional medical specialty organization representing Canadian physicians with special expertise in allergy and immunology and who are the preeminent experts in the diagnosis and management of allergic conditions, including vaccine allergy. The CSACI recognizes that the reports from the UK, along with the subsequent general recommendations, will undoubtedly and unfortunately lead to vaccine hesitancy. The CSACI would like to emphasize that the majority of individuals with a history of allergy will be able to safely receive vaccination for COVID-19.
The safety data in the clinical trials for the Pfizer/BioNTech vaccine for COVID-19 did not find a significant number of anaphylaxis events. As with any vaccine, the potential for adverse reactions, including allergic reactions, exists.
The NACI (National Advisory Committee on Immunization) has specifically identified polyethylene glycol (PEG) as a potential allergen in the Pfizer/BioNTech vaccine; however, the CSACI would like to point out that as of this date, PEG has not been confirmed as the cause of reaction for the reported adverse reactions in the UK. PEG is found in multiple products that are tolerated safely on a daily basis by many individuals in Canada, including bowel preparation products for surgical procedures, certain laxatives and other medications, certain skin care products and cosmetics, and some food and drinks. In addition, although allergy to PEG has been reported, it is reassuring to note that no cases of anaphylaxis to PEG in foods and drinks have been reported.
As such, the CSACI would like to commend Health Canada's prudent advice regarding the Pfizer/BioNTech vaccine for COVID-19, stating that ONLY those with known "…allergies to any of the ingredients in the Pfizer-BioNTech COVID 19 vaccine should not receive it…". Health Canada further recommends that individuals "who have experienced a serious allergic reaction to another vaccine, drug or food, …should talk to [their] health professional before [they] receive the vaccine".
The CSACI would like to reassure our fellow Canadians that unless one has a pre-existing allergy to a component of a vaccine, including the Pfizer/BioNTech COVID-19 vaccine, it is safe to proceed with vaccination for COVID-19. In addition, those with other allergic problems are no more likely to experience an allergic reaction to the COVID-19 vaccine than the general population and should safely be able to receive this vaccine—this includes those with a history of serious allergic reactions or anaphylaxis to substances that are not an ingredient in this vaccine, and those with food allergy, eczema, allergic rhinitis (hayfever), asthma, or stinging insect allergy.
We continue to monitor these reports closely and will continue to update our website, www.csaci.ca, as new information arrives.
About the Canadian Society of Allergy and Clinical Immunology (CSACI)
The CSACI is the largest national professional medical specialty organization in Canada representing physicians, allied health professionals and scientists with special expertise in the management of allergic and immunologic diseases. The Society is also dedicated to improving the quality of life of people with allergies through research, advocacy, continuing professional development and public education.
SOURCE Canadian Society of Allergy and Clinical Immunology - CSACI
