Exercise Shy? How to Improve Your Health Without Exerting Yourself Too Much
Exercise isn’t for everyone, and improving your health without breaking a sweat is still possible. It’s important, however, that you at least get some movement to preserve your well-being. If you’re exercise shy, these four methods will help you stay healthy without overexertion.
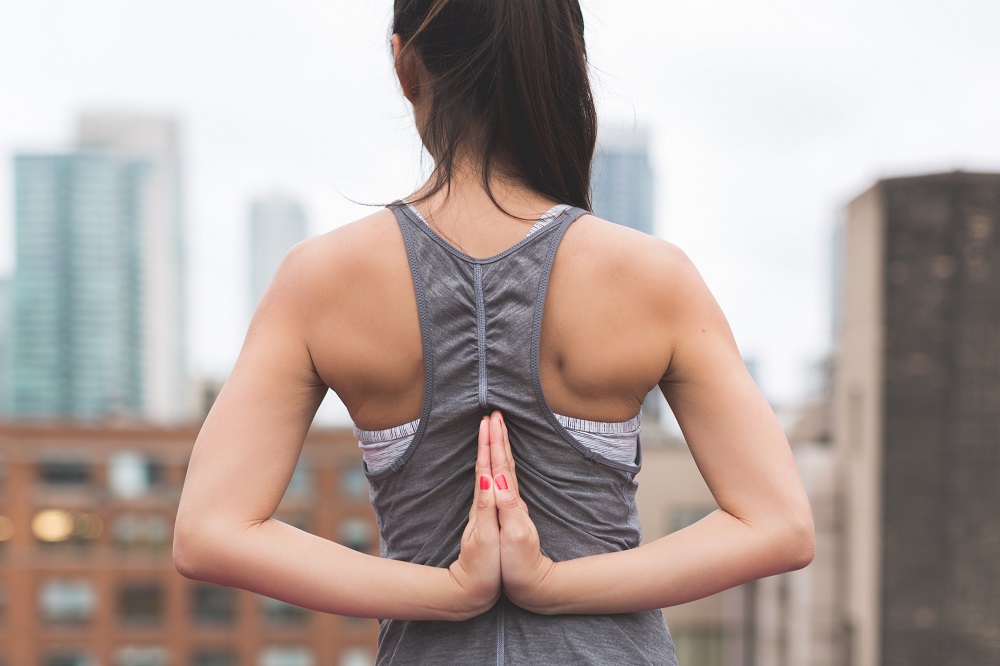
Try Aerial Yoga
Aerial yoga will give you the sensation of floating and help you forget that you’re even exercising. As explained by the Huffington Post, aerial yoga involves the use of a large silk hammock. This hammock is attached to a ceiling to suspend your body off the ground. While suspended, you’ll be performing different twists and stretches to work out your body. This form of yoga is also great for relieving stress.
Eat More Fish
Fish actually has the power to burn belly fat and help slim your figure. Fish is rich in protein, which burns calories when digested. The protein in fish can also help you stay fuller longer and prevent you from snacking on unhealthy foods. The omega-3 fatty acids found in fish further benefit you by stimulating protein synthesis. Salmon, halibut and sardines are among the best types of fish to eat for protein. Fish oil supplements are also known to increase protein synthesis and help with weight loss.
Soak in a Hot Tub
Believe it or not, the simple act of sitting in a hot tub has its health benefits. A Fox News article states that regular hot tub soaking for one hour at a time emulates the health effects of an hour-long, moderately difficult workout. The soothing hot water is able to reduce inflammation and regulate blood sugar levels. These benefits can help with weight loss. If it is no longer working, have your hot tub repaired with the right parts to start using it again.
Enjoy Spa Treatments
In addition to being relaxing, certain spa treatments can improve your overall health. CoolSculpting is a revolutionary treatment that’s designed to freeze fat cells and give you a slimmer physique. Some excess water weight may be eliminated with a body wrap. Aromatherapy using scents like vanilla, grapefruit and lemon can reduce unhealthy food cravings and help keep off the extra pounds. You can enhance your skin quality by getting a facial or salt scrub.
Living a healthy lifestyle while avoiding heavy workouts is possible with the right methods. Learning how to be good to your body without exercising a lot can help you live a more fulfilling life.
Digital Health Transformation in Action at HealthAchieve
The Intelligent Health Pavilion introduces four new partners
TORONTO, Nov. 3, 2017 The Ontario Hospital Association's annual signature event, HealthAchieve, is taking place next week on November 6 and 7 in Toronto. A unique learning and engagement experience for health care leaders, this year's event truly focuses on the future of health system transformation – where digital health is a key driver. With this in mind, we are introducing the Intelligent Health Pavilion (IHP) in partnership with the Intelligent Health Association (IHA).
"The Pavilion creates a platform for education and an opportunity for our health system partners to raise awareness around the adoption of new technologies in the health and wellness community," says Isabella Wai, Director, Commercial Partnerships, HealthAchieve. "We have 30 partners who are here to showcase how technology is improving patient care and safety while reducing costs."
HealthAchieve and the IHA are delighted to feature four new partners:
- Ontario Telemedicine Network (OTN) will display their innovative, new models of care in the home by way of the iHome Pavilion;
- Mi2 will share Mackenzie Health's journey to the smart hospital;
- Hamilton Health Sciences (HHS) will showcase their digitally connected hospital and home, where they are working hard to extend the hospital beyond the four walls of their sites; and finally,
- Mohawk College, one of the leaders in mHealth, together with MEDIC, will present Apps Alley.
"Our partners will also take to the stage in the Pavilion's Leadership and Innovation Theatres for several speaking sessions throughout the two days," says Harry P. Pappas, Founder & CEO, Intelligent Health Association. "Learn how these technologies are being seamlessly integrated to support caregivers and patients at each step of the health care journey."
None of this would be possible without the Intelligent Health Association, which is designed to showcase revolutionary technological advancements. We hope to see you at this world-class Pavilion where you can experience how technology is driving the future of patient care.
About HealthAchieve
HealthAchieve is more than an annual conference and trade show. It's an agent of change that drives the evolution of the health care system by focusing on the future. Global health care and business leaders come to HealthAchieve to be empowered by the potential that change holds. They seek new ways to push boundaries that move the health care system forward, to learn from and collaborate with industry leaders and innovators, and, ultimately, to change lives by helping to create a high-performing health system that is truly focused on putting patients first. Learn more about HealthAchieve online at www.HealthAchieve.com.
About the Intelligent Health Association
The Intelligent Health Association (IHA) is a not-for-profit, global organization founded to elevate awareness and to educate the life sciences community on the adoption of new technologies. Educationally focused, IHA is a vendor-neutral, technology and frequency agnostic association dedicated to promoting the use and adoption of auto-ID, NFC, RFID, RTLS, sensors and wireless technologies in the health care, assisted and independent living and nursing home industries. For more information, please visit: www.ihassociation.org.
SOURCE Ontario Hospital Association
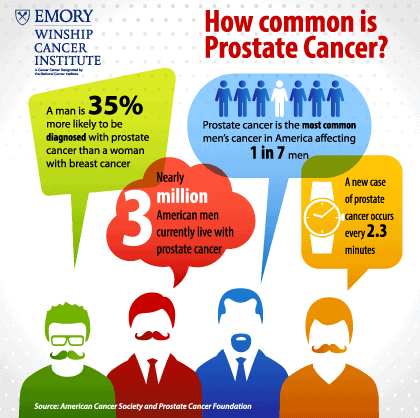
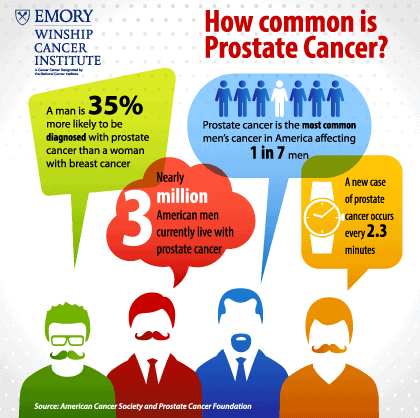
Does what you eat make you more likely to develop prostate cancer? If you have prostate cancer, are there foods that help fight it off and keep it from coming back? November is Prostate Cancer Awareness Month, a good time to focus on preventing one of the most common types of cancer in men around the world. Experts estimate that in the next 10 years, prostate cancer will be even more common than lung cancer. Early prostate cancer usually has no symptoms, so regular screening is important. Here are some things you can do to assess and reduce your risk.
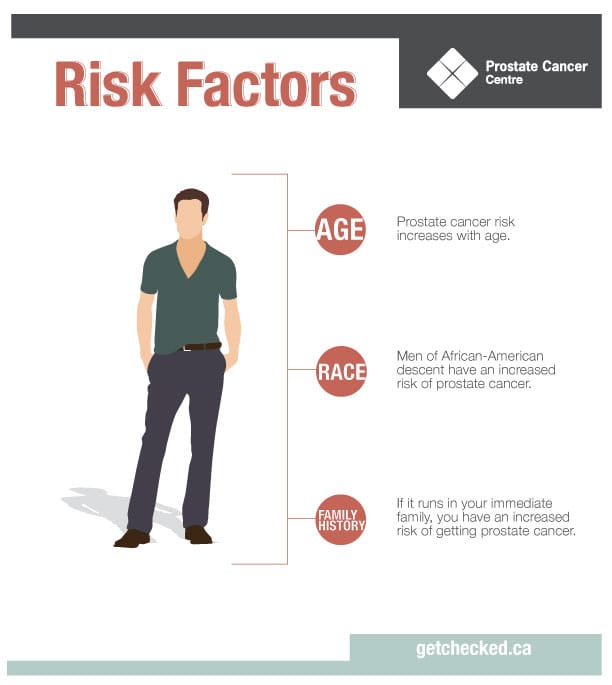
Are You at Risk?
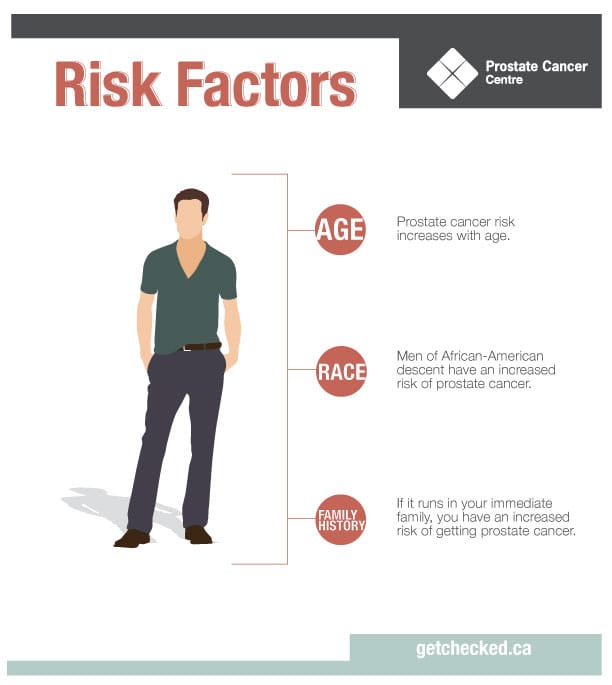
Men with a family history of prostate cancer are more likely to develop the disease. African American men are 1.6 times more likely than Caucasians to be diagnosed. Asian-American men and men who are Hispanic or Latino are less likely to develop prostate cancer.
The World Cancer Research Fund International conducted extensive studies on risk factors. They studied how diet, weight, and activity level affected risk. Here’s what they found.
- Strong evidence exists that men who are overweight or obese are more likely to develop prostate cancer.
- There is strong evidence that developmental factors contribute to increased risk. For example, the taller a man is, the higher his risk of developing prostate cancer.
- Beta-carotene was thought to reduce risk, but studies show that consuming large amounts of it has no effect on risk.
- Age is a factor. Men under 40 rarely develop prostate cancer, but the risk rises gradually after men reach 50.
- Geography matters. Men in North America, Europe, Australia, and the Caribbean islands are more likely to develop prostate cancer than men in Asia, Africa, and Central and South America are. Lifestyle differences such as a diet low in processed foods likely account for the difference.
- Diet plays a role. Men who eat a lot of red meat and high-fat dairy have a higher risk. These men also typically eat fewer fruits, vegetables, and whole grains.
Foods That Might Cause Prostate Cancer
Foods that are packaged and processed are often high in fat and calories. If you get it from a drive-through, it probably isn’t going to help you maintain a healthy body weight. Those foods aren’t just bad for your waistline; they might make you more likely to develop prostate cancer.
The Fred Hutchinson Cancer Research Center in Seattle studied men between the ages of 35 and 74. They found men who ate French fries, fried meats, or fried doughnuts once a week or more had a 30 to 37 percent higher risk of developing prostate cancer. Men with the lowest risk ate fried foods once a month or less. Saturated fats have been linked with heart disease, so avoiding them kills two birds with one stone.
Red meat contains heterocyclic amines (HCAs), carcinogens linked to several cancers. Stay away from processed beef, pork, lunch-meat, hot dogs, and sausage.
Prostate Protection Diet
Even if you only have one or two risk factors, healthy nutrition can help you prevent prostate cancer. Being overweight or obese is one of the biggest contributing factors to developing prostate cancer. Eating right and staying physically active helps keep your body mass index within a healthy range. Replace unhealthy foods with these options.
Nuts – Selenium is good for prostate health, and Brazil nuts contain 10 times your recommended daily allowance. Nuts also contain high levels of zinc, another mineral important to maintaining a healthy prostate. Nuts are high in protein, magnesium, and thiamin, all of which have health benefits.
Broccoli – Broccoli fights cancer. It is rich in sulforaphane, which helps the body detoxify itself and eliminates outside elements that may cause cancer. It also contains indole-3-carbinol, which suppresses cancer cell growth and lowers the production of protein specific antigen. One trial found men who eat broccoli more than once a week had a 45 percent less chance of developing advanced prostate cancer.
Cayenne – This bright red chili pepper contains capsaicin, which reduces pain and kills cancer cells. Capsaicin attacks cancer cells and causes them to self-destruct. It also fights atherosclerosis, prevents ulcers, and helps reduce your risk of diabetes.
Green tea – Men who drink at least three cups of green tea a day have a lowered risk of prostate cancer.
Pomegranates – Pomegranate extract slows prostate cancer cell reproduction and stops blood vessels from nourishing prostate tumors. Pomegranate juice is a great way to get it in.
Fish – Omega-3 fatty acids in fish both prevent prostate cancer and slow prostate tumor development. Eating fish can reduce your risk even if you’re genetically predisposed.
Fight Prostate Cancer and Make Money
It can be hard to eat healthy with today’s busy lifestyles. You can’t always find food that’s good for you. Vending machines offer convenient snacking, but they’re often full of the worst foods. Consider installing a Naturals2Go healthy vending machine at your office. Operators select inventory based on what their customers want and their own nutritional needs.
Offer nuts, bean chips, and all-natural fruit snacks in place of cookies and candy bars. Keep healthy options handy for yourself and those closest to you, and make money doing it. Contact us today to find out more about our machines.
New poll reveals Ontarians trust pharmacists with safe dispensing of medicinal cannabis
Pharmacist counselling of medicinal cannabis key to patient safety
TORONTO, Nov. 2, 2017 /CNW/ - With new polling data revealing Ontarians overwhelmingly trust their pharmacists to dispense medicinal cannabis in the province, the Ontario Pharmacists Association (OPA) is calling on the Government of Ontario to work with the federal government to update existing regulations to allow pharmacists in community pharmacies to safely dispense medicinal cannabis.
Polling commissioned by the OPA and conducted by independent polling firm CICIC Research, with a sample size of 800 respondents, reveals the following:
- A clear majority of adult Ontarians (70 per cent) agree medicinal cannabis should be dispensed by pharmacists;
- A majority of adult Ontarians (56 per cent) prefer that medicinal cannabis be dispensed by pharmacists, as opposed to other delivery methods; and
- Three-quarters of adult Ontarians agree that patients should be able to obtain medicinal cannabis products from pharmacists, so they can receive counselling and advice and can ask questions before receiving the product.
"I'm pleased to see Ontarians once again voice their trust in pharmacists to do more as trusted healthcare partners, this time by supporting pharmacists' ability to dispense medicinal cannabis to those who require it," said Andrew Gall, Chief Executive Officer of the OPA. "Local pharmacists in neighbourhoods across the province are highly trained and best positioned to provide face-to-face counselling to ensure the safe, appropriate and discreet access to medicinal cannabis."
A Role for Ontario's Pharmacists
Under existing regulations, a patient needs to be assessed by their healthcare provider and provided with a medical document for medicinal cannabis, after which they register directly with a licensed producer who processes their request and mails the product to the patient's home.
Unlike with other prescriptions, patients currently cannot access medicinal cannabis products at their local pharmacy. For Ontario's patients and the broader healthcare system, this is a missed opportunity and potential safety risk for a number of important reasons:
- Pharmacies are secure health centres that can monitor usage in real-time and properly store and handle sensitive products and controlled substances, such as medicinal cannabis. While mailing medicinal cannabis products directly to patients' homes seems convenient, safe and secure, pharmacies are found in practically every community across Ontario and remove any delays that mail-order introduces.
- As trusted healthcare professionals, Ontario's pharmacists can best support patient safety and education, and ensure appropriate access to medicinal cannabis. As medication experts within the patient's circle of care, pharmacists are in a unique position to help mitigate real or potential risks associated with medicinal cannabis, including identifying potential drug interactions and contraindications, and to suggest alternative therapies where appropriate.
Ontario's pharmacists are natural partners in the development of a patient-focused framework for the dispensing, tracking and monitoring of medicinal cannabis use and its effectiveness. The OPA will continue to advocate for enhancing patient safety, education and appropriate access to medicinal cannabis on behalf of its members.
Methodology:
Through independent research firm CICIC, OPA surveyed 800 respondents who self-selected to participate. An N of 800 is the typical sample size used for Ontario, and is absolutely considered reliable. Interlocking quotas based on age, gender and region were applied to ensure a representative sample of adult Ontario residents (age 18+).
Although telephone surveys are still being conducted, online research using self-selected participants is widely accepted as being valid research. It is an approach that is used by virtually every company in the industry. The margin of error for a sample of this size - if it were a probability (non-online) sample - would be +/- 3.5. All sample surveys and polls may be subject to multiple sources of error, including but not limited to, sampling error, coverage error and measurement error.
About the Ontario Pharmacists Association
The Ontario Pharmacists Association is the largest advocacy organization, continuing education, and drug information provider for pharmacy professionals in Canada.
We are dedicated to working on behalf of patients, pharmacists, pharmacy students, and pharmacy technicians across the province to evolve the practice of pharmacy and advocate for the highest standards of professional excellence and fair compensation.
We believe that by leveraging the unique expertise of pharmacy professionals, by enabling them to practice to their fullest potential, and by making them more accessible to all Ontarians, we will improve the efficiency and effectiveness of the province's healthcare system.
SOURCE Ontario Pharmacists Association
National Aboriginal AIDS Awareness Week 2017
Indigenous right to equitable health without discrimination or stigma
OTTAWA, Nov. 2, 2017 /CNW/ - The Canadian Aboriginal AIDS Network (CAAN) announces Indigenous leadership will gather on November 30, 2017 in Ottawa, ON for a Parliamentary Breakfast to launch Aboriginal AIDS Awareness Week 2017. It will be followed December 1 – 6, 2017 by events across the country (Vancouver, Edmonton, Regina, Winnipeg, Iqaluit, Toronto, and more) to unite an Indigenous response to HIV and AIDS in a parallel theme to international World AIDS Day: Right to Health.
This series of events across Canada will connect Indigenous organizations, government partners, health care providers, and community leaders as they reflect on what has been achieved and what must still be achieved by testing to "know your status", eliminating stigma and discrimination, and ensuring equitable access.
To end the AIDS epidemic, global efforts are aligned around a 90-90-90 Strategy which sets three measures of progress. On World AIDS Day 2016, the Government of Canada reported Canada's advances on these measures: 80% of HIV-infected people in Canada know their status; 76% of those who know they have HIV are on treatment; and 89% on treatment have suppressed viral loads.
"Indigenous communities hold the knowledge needed to close HIV target gaps, as we continue to be over-represented 2.7 times higher than other Canadians," said Ken Clement, CEO of Canadian Aboriginal AIDS Network. "Aboriginal AIDS Awareness Week is an opportunity for Indigenous Peoples, researchers, and policy makers to share wise and promising practices, learn from each other and build relationships across the country."
Right to Health is attune to the United Nations Declaration on the Rights of Indigenous People. Barriers exist to Indigenous Peoples' Right to Health including stigma, discrimination, and systemic racism. Indigenous communities hold strengths of traditional knowledge, culture, language and connection to land which supports wellbeing and health equity.
The Canadian Aboriginal AIDS Network and its launch day co-hosts, Canadian Global Health All-Parliamentary Caucus HIV TB & Malaria, Interagency Coalition on AIDS and Development (ICAD), and Pauktuutit Inuit Women's Association of Canada invite you to participate in Aboriginal AIDS Awareness Week as it brings awareness to the different aspects of HIV prevention and key populations such as Indigenous women and youth living with HIV and AIDS.
For Canada-wide schedule or to RSVP, visit: www.aboriginalaidsawareness.com
About CAAN www.caan.ca
The Canadian Aboriginal AIDS Network is a non-profit organization that leads a national forum for Indigenous Peoples to wholistically address HIV and AIDS, HCV, STBBIs, TB, mental health, aging, and co-morbidity issues; remedy social determinants of health through advocacy; and provide resources on these issues in a culturally relevant manner for Indigenous Peoples wherever they reside.
About ICAD www.icad-cisd.com/
About Pauktuutit http://pauktuutit.ca/
PHAC Budget Cuts Impact Indigenous HIV/AIDS Equity Access
Imbalanced Federal funding heavily emphasizes prevention, but underfunds care for People Living with HIV; disconcerting given indisputable evidence that support programs improve treatment adherence, drives down viral loads and eliminates further HIV transmission.
"In the case of CAAN, 2018 brings a 46% funding cut. The Public Health Agency of Canada's continued decision to severely reduce funding for CAAN decimates the leading voice of First Nations, Inuit, and Métis peoples living with HIV or AIDS and will have far-reaching consequences on both Indigenous health and reconciliation," stated Ken Clement, CEO of Canadian Aboriginal AIDS Network. "Over Aboriginal AIDS Awareness Week we hope to find ways to hold the process accountable and restore wellness opportunities for Indigenous Peoples."
SOURCE Canadian Aboriginal AIDS Network (CAAN)
Respect Your Universe collaborates with world renowned artists
(VANCOUVER, BRITISH COLUMBIA), OCTOBER 30, 2017 – RYU Apparel Inc. (TSX VENTURE: RYU.V; Frankfurt Stock Exchange: RYA) creators of urban athletic apparel, are pleased to present world-renowned artists, Jason Dussault and Raphael Mazzucco, in a collaborative effort titled, “No Home”. This blend of photography, paint, and mosaic tile work, embellished with a descriptive narrative crafted by celebrated poet, Prevail of Swollen Members, ushers in a powerful pictorial of a dystopian future. The thematic tone of the show reveals humanities deepest fears, and yet at the same time, highlights our collective strength and determination to survive.
“No Home” will be held on November 23 at the Chali Rosso Art Gallery at 549 Howe Street in Vancouver.
As a creative extension of Jason’s unique applications and garment work, a one of a kind collection between himself and RYU will debut one week later, November 28, at the company’s marquee downtown destination, located on Thurlow Street in Vancouver. These dynamic pieces are geared and designed to excite, elevating the wearer through a distinctive process focused on challenging classic concepts.
“When I was conceptualizing the message for ‘No Home’, I came to realize that it would be best presented alongside strong writing in the form of a short story” says Jason Dussault. “I turned to my longtime friend and partner, Prevail, to scribe some words to help guide the direction of the show. As a person of compassion and an artist of honesty, I am constantly challenged with the current state of affairs that we, as the human race, are faced with. When I came to Prevail for his help on ‘No Home’, I explained my concept and he instantly saw my greater vision. We have been working together on projects since the early 2000's. We have collaborated on everything from design, with my original custom clothing company Dussault, to my first gallery showing at the Hoerle Guggenheim in New York, where I was honored to be debuted alongside the legendary Retna.”
“Last year I was blessed to also have my works displayed in London at the Maddox Gallery, one of Mayfair’s premiere destinations for collectors around the globe. I was truly inspired when my mosaic and multimedia pieces were well received, and I was able to sell the entire collection to influencers from around the art world. As an artist I am constantly trying to challenge my understanding of different disciplines. For the first time, I have created jewelry, tools and costumes which have added to the profound medium of photography to my work. By including resin, ceramic and paint to my original images, I feel that I have broken new ground, and thus, have forged a new respect to the applications of art.”
-30-
About Jason Dussault
Represented by Hoerle-Guggenheim Contemporary Art Gallery in NYC and Maddox Gallery in Mayfair, London. Recent FC Barcelona commission to create a mosaic artwork of their coat of arms, where it was presented at the Rainbow Room in NYC and hand signed by all the soccer players. This was then put up for a Charity auction.
Last Solo show in NYC was a sellout, hosted by the late Glenn O’Brian editor of interview Mag and Warhol factory member.
Invited to do an Artist in residency for one month during the summer, at Ruschmeyer’s Hotel in Montauk, Long Island, NY. Jason worked at creating a series of vintage mosaic surfboards. Each work was created outdoors where hotel guests could interact with the artist and learn about the process. Each work was proudly presented at the end of the week.
Other achievements include:
- Invited to host an artist workshop and talk at the Soho House NYC.
- Rogers production of Reality TV show Dussault Inc
- Created the Iconic Dussault Hoodies
- Gene Simmons partnership
- Indy Car collaboration
jasondussault.com
About Prevail
As co-founder of Canadian rap group Swollen Members, Prevail has received 5 Juno awards, numerous Much Music Awards, and has sold nearly a million records worldwide over a career spanning two decades. Most recently, his wordsmithing has afforded him rare opportunities in the form of being a Ted X Vancouver presenter, an ambassador for the charitable organization Music Heals and creative speaking engagements with Finger Food Studios, and many others.
About Raphael Mazzucco
As a Canadian born fashion, art, and music photographer, Raphael has achieved an artist’s dream. He is inarguably one of the most important and influential photographers of our time. Having been featured in campaigns for Calvin Klein, Sports Illustrated, Victoria’s Secret, and Guess, his work is profound. A cameo on the famous show Entourage, also saw Raphael playing himself, conducting a portrait shot of the lead character for a book produced by Sean Puffy Combs and the legendary Jimmy Iovine. His works can be seen the world over and the clientele who have privately commissioned him for pieces are the crème de la crème of the collectors’ art world.
15 Doctor Recommended “To Do’s” to Fight the Flu

As we head into flu season there are many things we can do to “flu proof” ourselves. Regardless of whether you choose to get a flu vaccine or not, there are things we can do to heighten our chances of not getting sick this winter. Dr. Christopher Calapai, a New York based Osteopathic Physician board certified in family medicine, and anti-aging medicine provided us with a comprehensive list of 15 to do’s to fight the flu.
- Keep your surroundings clean, wipe surfaces at work, keep your cell phone clean. According to the CDC viruses can survive on a surface for up to 8 hours
- Wash your hands frequentlyand use a hand sanitizer. Remember the workplace and public spaces are a hotbed for germs. This is where the hand washing comes into play.
- Increase intake of vitamin D, C, E and A.Include foods such as red bell peppers (add to salads), sweet potatoes, chicken soup, salmon and garlic. Research shows that keeping vitamin D levels at 80 ng/ml or so decreases the risk of catching the flu and swine flu.
- Bring your own lunchto work where you can control food prep and ensure surfaces are clean.
- Get a full night's sleep.When you feel run down you're more susceptible to illness.
- Work from homewhen feeling sick. These days it's easier for people to work from home at the slightest signs of cold or flu.
- Eat kimchi!It’s delicious and a great probiotic which boost immunity.
- Add mushrooms to your meal.Packed with selenium they’re an immunity booster.
- Sip green or black tearich in polyphenols and flavonoids which ward off illness as well as L-theanine,
an immunity boosting amino acid. Green and black tea are also packed with polyphenols and flavonoids.
- Munch on sweet potato frieswhich are high in vitamin which helps us fight off bacteria and viruses.
- Don’t touch your face especially the eyes.The average person touches their face around 15 times
per hour! It’s something we do unconsciously so if we can be more aware of face touching the more we can stop.
- Soup it up!Chicken veggie noodle or ginger garlic soup fights flu and sinus infection.
- Exercise regularly!Doing 30 minutes of moderate cardio per day is optimal to enhance the performance of infection fighting white blood cells.
- Go hands free on the smartphone.When we put our phones down and then pick them up or touch them this is where viruses can spread. Using earbuds and cleaning the phone with a devise friendly cleaner will help.
- Lose the booze.You really want to cut back on alcohol consumption during flu season. It dehydrates us and lowers our immunity so our ability to fight off virus is impaired.
About the Doctor:
Dr. Christopher Calapai, D.O. is an Osteopathic Physician board certified in family medicine, and anti-aging medicine. Proclaimed the "The Stem Cell Guru" by the New York Daily News, Dr. Calapai is a leader in the field of stem cell therapy in the U.S. His stem cell treatments have achieved remarkable results in clinical trials on patients with conditions as varied as Alzheimer's, arthritis, erectile dysfunction, frailty syndrome, heart, kidney and liver failure, lupus, MS and Parkinson's. He has worked with Mike Tyson, Mickey Rourke, Steven Seagal, and Gotham's, Donal Logue; and as a medical consultant for the New York Rangers. Connect with him via twitter @drcalapai or at www.drcal.net
5 Healthy Foods for the Women of All Ages
Every woman needs to take the required nutrients for good health. Although eating the right diets are good for both sexes, but women have their own specific dietary requirements. According to research, when women eat the right things, they will live better and happier.
Here are 5 healthy foods for women of all ages. They have been tested and trusted to be effective in boosting feminine immune systems.
Cranberries
Studies have proven that the advantage of cranberries can never be overemphasized. Among other things, it reduces the risk of urinary tract infections, heart disease and breast cancer. Healthcare professionals recommend every woman should take at least one glass of juice daily. It nourishes their skin and boosts their immune systems.
Oats
High cholesterols can give rise to building up of plaque in your artery walls. However, if it is left untreated, it can lead to other ailments such as stroke and heart attack. Stroke and heart attack are among the killer diseases in most American women.
The good news is that it is difficult to combat; you can handle the situation effectively by eating healthy diets that includes oatmeal, fiber-rich whole grains etc. Oats can perfectly protect you against various forms of heart diseases.
Oats are filled with amazing nutritional benefits, and they are truly great for female health. They can aid digestion, stabilize blood pressure, wards off potentially dangerous dips in glucose and derailing hunger and keep your heart healthy.
Oats contains vitamin B6, which aids in the prevention of mood swings, birth defects in children and PMS. Overall, women are recommended to eat oats both during and after pregnancy.
Milk
One of the major health challenges that women face around the world is calcium deficiency. Regular intake of milk is highly recommended in women of all ages. If possible, try and combine the milk with vitamin D, it will help in keeping osteoporosis at bay. Milk prevents women from all symptoms of the killer PMS.
Further studies shows that milk helps in building up a woman’s nerves, muscles, teeth and bones. If you don’t take enough milk, it can lead to osteoporosis, thereby causing brittle and weak bones. Milk is the main source of calcium.
Drinking milk both during and after childbirth helps the woman to remain healthy and energetic. According to research, almond milk is more effective in women than whole drink especially during pregnancy.
Dark chocolate
Dozens of research shows that chocoholics or people who consume more of dark chocolates stay in better shape than those who don’t take it. Another study in the Circulation Heart Failure journal discovered that women that take about one or two servings of quality chocolates per week had 32% risk of developing heart failure than those who bluntly refused to take cocoa.
Further studies shows that cocoa contains anti-inflammatory compounds, flavanols and polyphenols, which helps in protecting the heart. When you are buying dark chocolate, ensure you take the one that contains about 74% or more cocoa solids, due to their flavanol-rich compounds.
Mushrooms
Studies shows that mushrooms are best dietary sources. Women are recommended to take about half cup of it on a daily basis. Mushrooms are rich with potassium; they can offset all negative effects of excess sodium, as well as lowers your blood pressure levels. Another study at the University of Florida says that people who eat at least 4 ounces of cooked mushrooms daily for about 4 weeks, develops increased immunity and boost greatest concentration than those that don’t.
Author Bio:
Ryan Varela is the CEO of Boost Health Insurance which provides customized and affordable health care plans for thousands of customers across the United States. Ryan has nearly a decade of experience in the health care industry and continues to serve the greater need to educate and deliver access to affordable options to those who need health care the most.
The clocks fall back, but you don't have to.
When we turn our clocks back an hour on Sunday, November 5, Canadians get an extra hour of sleep in the morning and a lot less light in the evenings. It's more important than ever to find time for regular exercise, and the week after the time change is a good time to get started.
According to Abby Johnson, team training specialist with GoodLife Fitness, exercise offers many benefits when it comes to adjusting to time changes, sleep interruptions and colder, darker days.
Exercise can:
Reset circadian rhythms – The switch out of Daylight Savings time can interrupt your sleep patterns for up to a week. Exercising at the same time each day can help you get your sleep back on track after the time change
Improve mood – With fewer daylight hours, many Canadians feel their energy and mood decline. In fact, as many as 15 percent of Canadians will suffer from seasonal affective disorder (a form of depression) in their lives. Regular exercise causes your brain to release feel-good hormones that can help regulate and improve mood.
Boost energy – More darkness, colder temperatures, and sleep disruption can leave us feeling distracted and lazy. It’s tempting to stay indoors and watch TV, eat and drink more and be less active. But physical activity increases heart rate, circulation, and mental focus. Regular workouts will leave you feeling energetic, stronger and more focused.

Johnson suggests connecting with a personal trainer or other fitness experts to brainstorm ways to use the fall time change to kick-start your winter health. Here are some ideas.
Use the extra hour to work out. This may be the only time in the year you wake up BEFORE the alarm. Channel the time change to build in some exercise. Commit to exercising in the morning for one week and see if it becomes a habit. Also, it will be light for the first few weeks, and easier to get to the gym or out for a run.
Don’t be deterred by darkness. Increase your exposure to bright light and physical activity during the day until late afternoon/early evening to help compensate for the overall reduction of daylight hours. Take advantage of morning and lunchtime to go for a run, bike to work, or get your co-workers together for a lunchtime walk to enjoy more sunshine and fresh air. During winter months, remember to take a vitamin D supplement.
Change your body and your outlook. Change your posture by pushing your shoulders up and back, take deeper breaths, look ahead. Keep moving, whether it’s walking to work, jogging in the morning, taking the stairs or playing outside with your kids.
Stay hydrated and choose healthy foods. Avoid caffeinated beverages, since too much caffeine can further disrupt your natural sleep rhythm.
Fit in full-body fitness moves. Exercises that use various parts of your body can kick-start your metabolism and give you more energy. Here are some examples of full-body moves to boost energy:
Superman: Lie face down and extend arms and legs. Flutter-kick legs up and down, simultaneously reaching arms toward feet, then back overhead. That’s one rep. Do 2 or 3 sets of 10.
Goblet squat with a press: Hold a hand weight vertically; lower hips, bringing elbows inside knees. Return to standing and press arms overhead. That's 1 rep. Alternate sides with each rep. Do 2 or 3 sets of 10.
Single leg deadlift: Hinge at the hips, lowering torso as right leg lifts. Working balance, try to touch fingertips to the floor, then come back to start. That's 1 rep. Do 2 or 3 sets of 10 on each side.
We can connect you with a personal trainer in your area who can discuss the best way to tackle the time change with exercise, as well as show some quick energy boosting workouts to tone your body, engage your heart and make you more alert. Please let me know if you’d like to book an interview.
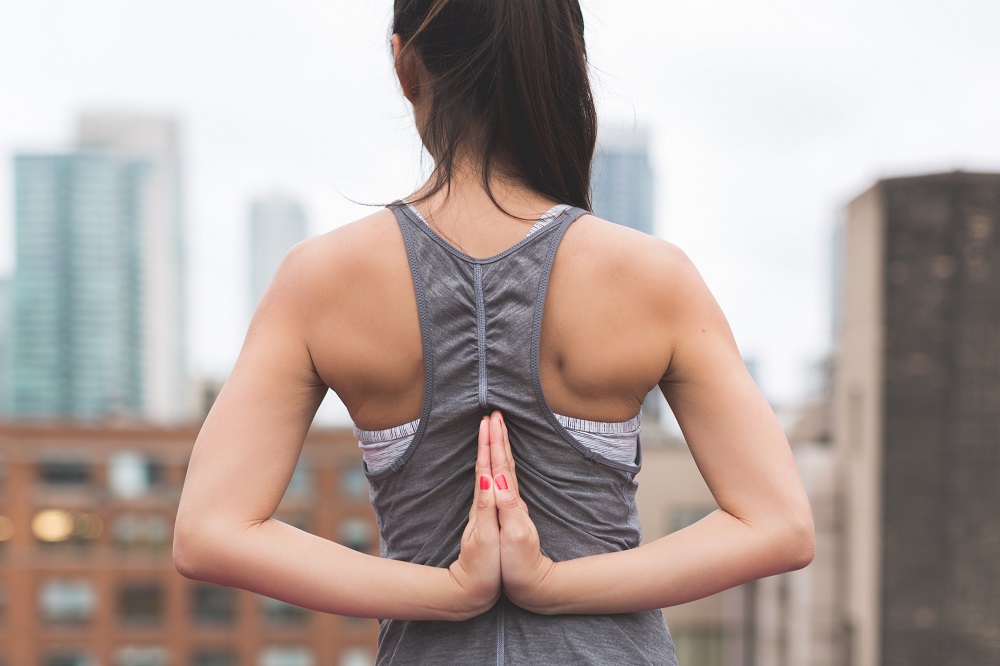
Skins RY400 Recovery Long Tights and Long Sleeve Top

Some time ago Skins reached out to me and wanted to send me both tights and a top. I did some research on their products and agreed. Not only because I am a competitive athlete but I am a strong believer in recovery; recovery is very crucial when you put your body through high intensity training. If you are not fully recovering between workouts you will peak and not be able to perform at your best.
After reading up about the benefits of Skins recovery leggings and long sleeve top I figured I would give them a try. After my workout I through on my leggings and long sleeve shirt, skins recommends that you wear your recovery clothes for a minimum of 3 hours after your exercise allowing you to circulate blood faster feeding your muscles more oxygen.
The next day I did notice what I wasn’t as sore as I typically would be. As for comfort level the leggings were super flexible, and the elasticity was durable and held up making it easier by not having to constantly pull up. The long sleeve shirt sat perfectly around my neck and wasn’t too high as some long sleeves are. I definitely recommend Skins recovery line to any athlete to help speed up recovery.
Interested in learning more? Click the link below:
Yellow-Compression Guide_Original
If you're interested in snagging yourself a pair check them out:
https://www.skins.net/usa/skins-ry400-womens-long-tights.html
https://www.skins.net/usa/skins-ry400-womens-top-long-sleeve.html