5 Reasons Why More and More People Are Saying ‘No Way’ to Valentine’s Day
Whether you’re in a couple or rolling solo, Valentine’s Day comes with expectation and pressure. With #CoupleGoals as a consistently trending hashtag, countless pictures of couples on social media, the obsession of celebrity break ups and make ups and TV shows like the Bachelor and Bachelorette serving up contrived romance sprinkled with drama, the way we think of love and romance has changed. Dr. Sanam Hafeez, a New York Board Certified Neuropsychologist explains why so many people say ‘no way’ to Valentine’s Day and offers some alternatives that shift this negative mindset.
- “Valentine’s Day is a ‘Hallmark Holiday’ and I’m still broke from Christmas.”
When money is tight many people may want to cut back on spending especially for things they feel are frivolous. “Financial stress is a common thing and when people are made to feel pressured to spend, they get resentful and want to claim their power,” explains Dr. Hafeez. Instead of boycotting all romance, put a $20 maximum on gifts and you’ll see how sweet, thoughtful and creative you can get.
- “Every restaurant is crowded and the service is terrible.”
Nothing kills romance faster than crowds and a bad experience dining out. Since everyone goes out to eat on Valentine’s Day there will be a lapse in service. “One way for couples to celebrate is to call their favorite restaurant in advance and have a meal prepared they can pick up and heat up at home,” suggests Dr. Hafeez. “You can either break out the fancy dishes and dress up or you can put on sweats and eat while watching a movie, the important thing is that you enjoy yourselves and aren’t stressed,” she adds.
- “We’ve been together for ages. Every day is Valentine’s Day! Do we really need to celebrate?”
“Celebrations and traditions are important in a relationship and when they fall away it’s usually a sign of trouble and disconnection. While you may not feel the need to do anything extravagant use the day to appreciate the love you have and life you’ve created, even if it’s in a small way,” Hafeez advises.
- “I’m single so what’s the point?”
Rolling solo on Valentine’s Day again, all the more reason to turn it into a Self Love Day. Being single on Valentine’s Day can be tough for people, especially those still healing from a break up or divorce. “You want to really be kind and caring to yourself. Booking a massage, getting a haircut, or arranging a single ladies night with your single friends could be just what’s needed. Focus on creating your own happiness,” says Dr. Hafeez who often sees a link between break up depression and anxiety over holidays.
- “I’m just to busy for love and romance and all that stuff.”
Some people are just focused on other things that are top priority in their lives. There are plenty of women who are turned on more by generating income for their businesses than concerning themselves with outside approval or validation. There has been a rise in female entrepreneurship with more millenials and Gen X’ers preferring to build empires than romantic relationships. For them it’s just February 14th the mid way point to a short month. “There’s nothing wrong with women wanting to focus on their professional lives. They often feel to focus on business, romance, which may cause them to lose focus, has to be shelved for a while, this is more common these days,” Dr. Hafeez shares.
While many say ‘no way’ to Valentine’s Day there are millions saying I DO.
According to a 2017 survey of 1000 people done by James Allen, an online diamond and bridal jewelry retailer, 43 percent of millennials say Valentines Day is their top pick for proposal day. November – February is considered proposal season.
Some other mind-blowing stats that clearly show Cupid isn’t going away anytime soon are.
In 2017, the National Retail Federation put the estimated total spending at over $18.2 billion. That's an average of $136.57 per person.
Jewelry is the most popular gift with 20 percent of consumers expected to buy jewelry, with a total of $4.3 billion on bling, the NRF said.
$2 billion will be spent on flowers, with roses being most popular. 250 million roses are produced for the holiday, the Society of American Florists said.
The American Greeting Card Association puts that industries pay out at 1 BILLION… yes folks $1 … for paper.
About Dr. Sanam Hafeez:
Dr. Sanam Hafeez PsyD is a NYC based licensed clinical neuropsychologist, teaching faculty member at the prestigious Columbia University Teacher’s College and the founder and Clinical Director of Comprehensive Consultation Psychological Services, P.C. a neuropsychological, developmental and educational center in Manhattan and Queens.
Dr. Hafeez masterfully applies her years of experience connecting psychological implications to address some of today’s common issues such as body image, social media addiction, relationships, workplace stress, parenting and psychopathology (bipolar, schizophrenia, depression, anxiety, etc…). In addition, Dr. Hafeez works with individuals who suffer from post traumatic stress disorder (PTSD), learning disabilities, attention and memory problems, and abuse. Dr. Hafeez often shares her credible expertise to various news outlets in New York City and frequently appears on CNN and Dr.Oz.
Connect with her via twitter @comprehendMind or www.comprehendthemind.
Groundbreaking report looks at Canadian cancer care exclusively from the patient perspective
Report highlights significant challenges for many from fearing something is wrong through to finding a "new normal" after cancer treatment is over, and beyond
TORONTO, Jan. 29, 2018 /CNW/ - The Canadian Partnership Against Cancer has released Living with Cancer: A Report on the Patient Experience. This groundbreaking report reflects the voices of over 30,000 Canadians and is the country's largest accumulation of patient data on the experiences of people living with, and beyond, a cancer diagnosis.
The report shows that while their cancer may be well treated, many patients experience significant, and often debilitating, physical and emotional side effects of the disease that are often not being adequately addressed.
Quick facts
- Up to one in five cancer patients report no one discussed different treatment options for their cancer with them.
- Up to one in four report that their care providers did not consider their travel concerns when planning for treatment.
- One in four report that they were not satisfied with the emotional support they received during outpatient cancer care.
- Eight in 10 report having physical challenges after their treatment ends. Increased fatigue and changes in sexual function and fertility were the biggest concerns.
- Seven in 10 report having emotional challenges after treatment ends. Worry about cancer returning, depression and changes in sexual intimacy were their biggest concerns.
- Four in 10 report having practical challenges after their treatment ends. Returning to work and school, as well as financial problems such as paying health care bills and getting life insurance were the biggest concerns.
View the full report
To address these gaps in the cancer patient experience, the Partnership is pushing for change collaborating with provincial governments, cancer agencies and programs, and other health sector organizations to implement tools that allow patients to report details of their symptoms in real time to their doctors. Doctors can then use this information to promptly refer patients to therapists or other services where their symptoms can be managed. This information can also be used for planning at the system level to ensure services are available where they are needed.
Efforts to improve the cancer patient experience
This report, and efforts to directly address patient needs, would not be possible without ongoing, multi-year investments by the Partnership and provincial cancer programs across the country. The Patient Reported Outcomes (PRO) initiative started in 2013 pushing for all jurisdictions in Canada to have a measurement and reporting cycle for the cancer patient experience. Gaps are now being recognized and through a coordinated pan-Canadian approach, most provincial cancer programs have implemented tools to screen for patient distress, which allows for patients to report, at the time of their medical appointment, on symptoms they are experiencing including: pain, fatigue, anxiety and depression.
In total, eight provinces over five years have implemented systems that collect real-time feedback from patients, at the point of care. This feedback supports immediate discussions with health care professionals that can lead to more meaningful solutions to common problems faced by cancer patients. This means that the additional burden to be proactively tracking and reporting on issues, while competing for the time of medical staff, has been lifted off of the patient. The responsibility is now placed on the health care provider to use standard tools and practices to routinely respond to patient concerns. Next, the Partnership and provincial cancer programs will work to close the gaps highlighted by patients and will continue to measure if improvements in patient needs are being achieved. The initiative will be expanding to other provinces and territories in the next five years.
Quotes
"All too often, as soon as the word 'cancer' is spoken, the focus is on the disease and not the person. But the survivor's experience with cancer does not end when the disease is gone. This report from the Canadian Partnership Against Cancer shines a light on how to better support patients before, during and after treatment."
Ginette Petitpas Taylor
Minister of Health
"Following my cancer treatment, I felt like I was left floating in the breeze in a scary world of uncertainty. I was no longer actively fighting against my tumour but I had this underlying fear that it might recur at some point," said Charlotte Kessler, patient advisor for the Partnership. "My doctors never told me I was in the transition phase of my cancer experience, they did not discuss next steps and things I could expect, and they did not direct me to any resources. I felt like I was on my own," said Charlotte who is also featured in the report.
"Findings from this report suggest a greater need for people with cancer to speak with their family doctor or oncologist about their concerns before, during, and after treatment," said Cindy Morton, CEO of the Partnership and cancer survivor. "Patients should not assume their concerns are normal, even if told so, and should discuss symptoms with their doctor. The health system must also do more to support doctors with the right tools and resources to get patients the care they need."
"This important report highlights the experience of having cancer in Canada, the many kinds of support people need and where the gaps are, right from diagnosis through treatment and beyond," said Lynne Hudson, President and CEO, Canadian Cancer Society (CCS). "We all need to do a better job of meeting the needs of Canadians with cancer so patients feel supported and informed throughout their cancer journey. At CCS, we have programs and services in place for cancer patients and their families – including providing reliable information, peer support programs and transportation services – but more needs to be done. We look forward to working with the Partnership and other partners in the health sector to use the information in this report to better service Canadians affected by cancer."
"As the survey data show, many patients continued to suffer symptoms like pain, fatigue and depression without being referred to services that could have helped them like physiotherapy or psychotherapy," said Esther Green, Director, Person-Centred Perspective at the Partnership. "The findings suggest health care providers need to have meaningful discussions with their patients to assess their emotional, physical and practical concerns following cancer treatment and refer them to the appropriate supports. This is not always happening. Not for a lack of concern by doctors for their patients but because of inadequate tools, resources and other supports needed at the system level."
A full copy of the report is available at systemperformance.ca.
Data for Living with Cancer includes data from multiple sources, including Patient Reported Outcomes partners, the Ambulatory Oncology Patient Satisfaction Survey and initial results from the first Canada-wide study of cancer survivors.
About the Canadian Partnership Against Cancer
As the steward of the Canadian Strategy for Cancer Control, the Partnership works with partners to reduce the burden of cancer on Canadians. Our partner network – cancer agencies, health system leaders and experts, and people affected by cancer – brings a wide variety of expertise to every aspect of our work. After 10 years of collaboration, we are accelerating work that improves the effectiveness and efficiency of the cancer control system, aligning shared priorities and mobilizing positive change across the cancer continuum. From 2017-2022, our work is organized under five themes in our Strategic Plan: quality, equity, seamless patient experience, maximize data impact, sustainable system. The Partnership continues to support the work of the collective cancer community in achieving our shared 30-year goals: a future in which fewer people get cancer, fewer die from cancer and those living with the disease have a better quality of life. The Partnership was created by the federal government in 2007 to move the Strategy into action and receives ongoing funding from Health Canada to continue leading the Strategy with partners from across Canada. Visit www.partnershipagainstcancer.ca.
SOURCE Canadian Partnership Against Cancer
Bell Let's Talk and The Rossy Family Foundation commit $1 million to develop a national standard for post-secondary student mental health
- New standard to establish mental health best practices at Canadian universities, colleges and institutes to support student mental health and academic success
- Standard will be developed in collaboration with students, staff and faculty
- The Rossy Family Foundation and Bell Let's Talk each donating $500,000
MONTRÉAL, Jan. 29, 2018 /CNW Telbec/ - Bell Let's Talk and The Rossy Family Foundation (The RFF) today announced a joint $1,000,000 donation for the creation of a national standard for post-secondary student mental health to support student success on campuses across Canada. The RFF and Bell Let's Talk have engaged the Mental Health Commission of Canada (MHCC) to lead the project to establish the standard in collaboration with Canada's standards setting organizations.

"The success of the National Standard of Canada for Psychological Health and Safety in the Workplace set the stage for this new initiative. We believe there is tremendous potential to improve the lives and academic success of Canada's post-secondary students by taking a similar systematic approach," said Mary Deacon, Chair of Bell Let's Talk. "Colleges and universities throughout the country are working hard to ensure a psychologically healthy and safe environment for their students. As with the workplace standard, they will benefit from a nationally established, systematic framework to guide and facilitate their mental health efforts."
"Post-secondary education is an exciting time as youth stretch their wings and become more independent," said Louise Bradley, President and CEO of the Mental Health Commission of Canada. "It is also a time of increased susceptibility to mental health problems and illnesses as students juggle financial, academic, family and personal demands. The Mental Health Commission of Canada is pleased to work with our partners to develop a standard that will provide a roadmap for educational institutions as they strive to safeguard and promote student mental health."
"The health and well-being of students is a priority for Canada's universities and we applaud Bell's leadership and commitment on this important initiative," said Paul Davidson, President of Universities Canada. "We look forward to working with Bell Let's Talk, The Rossy Family Foundation, the Mental Health Commission of Canada and others to ensure that students, staff and faculty are well-supported."
"Providing a positive and healthy learning environment for all has always been a priority for Colleges and institutes across Canada," said Denise Amyot, President and CEO of Colleges and Institutes Canada. "As the national conversation on mental health has evolved over the years, they have always been at the forefront and have worked diligently to continually improve their services and support their students. Colleges and Institutes Canada is thrilled to be a partner as our members and their students will benefit immensely from this national standard for post-secondary student mental health, which will help all Canadian post-secondary institutions share and access best practices from across the country."
A national standard for post-secondary student mental health will create a practical and flexible framework that enables institutions to protect and promote students' psychological health and safety. Like the workplace standard, it will provide guidance for Canadian universities, colleges and institutes to promote student success through a collaborative approach to mental health between staff, faculty and students.
Of the more than 2 million people enrolled in Canadian post-secondary institutions, almost 70% are 24 or under, a demographic particularly susceptible to developing mental health issues. Research by the US National Institute of Mental Health has shown that 75% of people with a mental health disorder receive their first diagnosis between 16 and 24. Canada's National College Health Assessment Survey found 32% of students have been diagnosed or treated for anxiety or depression in the previous year.
At the same time, young people are more engaged when it comes to mental health than ever before, with 87% saying they are more aware of mental health issues than 5 years ago, according to research conducted by Nielsen last October.
Bell Let's Talk helped fund the development of the National Standard of Canada for Psychological Health and Safety in the Workplace in 2013, and was one of the first organizations to adopt the standard. The new post-secondary standard aims to establish a similar evidence-informed, systematic approach to addressing mental health, a practical and flexible framework that individual institutions can adapt to their unique environments.
Bell Let's Talk Day is January 31
We invite everyone to take part in the mental health conversation on Bell Let's Talk Day. Bell will donate 5 cents to Canadian mental health programs for each of these interactions on January 31, at no extra cost to participants:
- Text and talk: Every text message, mobile and long distance call made by Bell customers
- Twitter: Every tweet using #BellLetsTalk including a Bell Let's Talk hashtag emoji and Bell Let's Talk Day video view
- Facebook: Every view of the Bell Let's Talk Day video at Facebook.com/BellLetsTalk and use of the Bell Let's Talk frame
- Instagram: Every Bell Let's Talk Day video view
- Snapchat: Every use of the Bell Let's Talk filter and video view
Bell Let's Talk Day 2017 set all new records with 131,705,010 messages, growing Bell's funding for Canadian mental health by $6,585,250.50. #BellLetsTalk was Canada's top hashtag in 2017, and is now the most used Twitter hashtag ever in Canada.
With approximately 729,065,654 interactions by Canadians over the last 7 Bell Let's Talk Days, Bell's total commitment to mental health, including an original $50-million anchor donation in 2010, has risen to $86,504,429.05. Bell expects its donation commitment to reach at least $100 million in 2020. To learn more, please visit Bell.ca/LetsTalk.
About The Rossy Family Foundation
The Rossy Family Foundation is a Montréal-based philanthropic foundation that funds initiatives in mental health, health care, education, the arts and Canadian civil society.
About the Mental Health Commission of Canada
The Mental Health Commission of Canada is a catalyst for change. We are collaborating with hundreds of partners to change the attitudes of Canadians toward mental health problems and to improve services and support. Our goal is to help people who live with mental health problems and illnesses lead meaningful and productive lives. Together we create change. The Mental Health Commission of Canada is funded by Health Canada.
The International Day of Zero Tolerance for Female Genital Mutilation is a United Nations sponsored annual awareness day that takes place on February 6 as part of the UN's efforts to eradicate female genital mutilation. FGM involves removing and damaging healthy and normal female genital tissue, and interferes with the natural functions of girls' and women's bodies.
Lucinda E. Clarke, author of the suspenseful literary fiction, Amie Cut for Life (Umhlanga Press), which deals with FGM and human sex trafficking, is available to discuss essential aspects of FGM with your audience – the what, who, where, why and how – as well as why the International Day of Zero Tolerance is so important.
OVERVIEW OF FEMALE GENITAL MUTILATION:
WHY
The practice, rooted in gender inequality, attempts to control women’s sexuality and ideas about purity, modesty and beauty. It is usually initiated and carried out by women (!), who see it as a source of honor, and fear that failing to have their daughters and granddaughters cut will expose the girls to social exclusion.
The reasons why female genital mutilations are performed vary from one region to another as well as over time, and include a mix of socio-cultural factors within families and communities. Where FGM is a social convention (social norm), the social pressure to conform to what others do and have been doing, as well as the need to be accepted socially and the fear of being rejected by the community, are strong motivations to perpetuate the practice. In some communities, FGM is almost universally performed and unquestioned.
FGM is often considered a necessary part of raising a girl, and a way to prepare her for adulthood and marriage.
FGM is often motivated by beliefs about what is considered acceptable sexual behaviour. It aims to ensure premarital virginity and marital fidelity. FGM in many communities is believed to reduce a woman's libido and therefore it will help her resist extramarital sexual acts. When a vaginal opening is covered or narrowed, the fear of the pain of opening it, and the fear that this will be found out, is expected to further discourage extramarital sexual intercourse among women with this type of FGM.
FGM is more likely to be carried out where it is believed that being cut increases marriageability.
WHERE
Female genital mutilation is widely practiced in Africa, Asia and the Middle East. However with many people now making their home is new countries, the practice is now seen in North America (USA and Canada) and most countries in Europe – despite it being illegal. Children are often sent overseas to their country of origin for the procedure during the school holiday (the cutting season). UNICEF estimated in 2016 that 200 million women living today in 30 countries have undergone the procedure. Since 1990, the estimated number of girls and women in the US who have undergone or are at risk of the practice has more than tripled.
SOME OF THE DANGERS
The procedure can cause bleeding (haemorrhage), chronic pain, scar tissue and keloid, recurrent infections (eg tetanus), swelling of the genital tissue, fever, wound healing problems, difficulty urinating and passing menstrual flow, the development of cysts, an inability to get pregnant, sexual problems, complications during childbirth, infant mortality, shock and even death.
This does not even touch the damage to the dignity and self-esteem of the victim.
More than 40,000 Ontarians were newly started on high-dose prescription opioids in 2016
TORONTO, Jan. 25, 2018 /CNW/ - More than 40,000 Ontarians were newly started on high doses of prescription opioids (over 90 mg of morphine per day, or the equivalent dose of a different opioid) in 2016. This is despite evidence that those who receive prescription opioids at higher than recommended doses are several times more likely to overdose compared to those on lower doses.
In addition, according to Starting on Opioids, a new report by Health Quality Ontario, the provincial advisor on health care quality, 1.3 million people overall were started on opioids in 2016 – at any dosage. This is a slight decrease of about 25,000 new starts, or 2%, from 2013.
"At current rates of decrease, it would take Ontario more than a decade to reach the same prescribed opioid consumption rates as other economically similar countries such as Australia and the U.K.," says Dr. Joshua Tepper, President and CEO of Health Quality Ontario. "We are hopeful the intervention of initiatives currently underway in Ontario to change opioid prescribing practices will bring the rate down much faster."
The report also shows that of the 1.3 million Ontarians started on opioids at any dosage, nearly 325,000 were started with a prescription for more than 7 days. Evidence tells us that initial prescriptions for more than 7 days of opioids have been associated with a higher risk of long-term use.
Starts of opioids, as defined in the report, are prescriptions for people who have not filled an opioid prescription in at least six months.
"We encourage prescribers and patients to consider if there are non-opioid therapies that might be useful, before prescribing opioids," says Dr. Tepper. "If opioids are the best option, the current standards and guidelines encourage the lowest possible dose and a short duration."
For acute pain, a duration of 3 days or less is often recommended, according to expert opinion. And for starting on opioids for chronic pain, standards and guidelines say it's preferable not to exceed a dose of 50 mg of morphine or equivalents per day, and to initiate opioids only after other therapies have been tried.
"It should be emphasized that chronic pain is very difficult to manage. For example, patients may not be able to afford non-opioid therapies, such as physiotherapy," says Dr. Tepper. "And given the overdose crisis, which is increasingly related to non-prescription heroin and fentanyl, it is also very important for prescribers to not suddenly discontinue prescription opioids so patients don't turn to street sources."
To reduce the risk of addiction and opioid poisoning, there are some encouraging initiatives underway across the province to improve the prescribing of opioids.
In recognition of troubling trends in opioid prescribing and increasing opioid-related deaths, in 2016, the Ministry of Health and Long-Term Care launched a comprehensive strategy to address opioid-related harms, with a focus on modernizing opioid prescribing and monitoring, improving access to pain treatment, and enhancing addictions supports and harm reduction.
At the request of the Ministry of Health and Long-Term Care, Health Quality Ontario, in collaboration with patients, health care providers, caregivers, and organizations across the province, is in the final stages of developing three quality standards, that outline for clinicians and patients what high-quality care looks like. Two are about opioid prescribing for acute pain (short-term) and chronic pain (long-term), with a third outlining how to identify and treat people with opioid use disorder.
These standards of care will be put into action through coordinated efforts with a number of health care organizations who are providing customized data, tools and supports to physicians for appropriate prescribing.
Other initiatives are underway to prevent opioid addiction and overdose. To name a few, there are various hospitals designing programs to help with the post-discharge period for patients who have had major surgery to better manage their pain, and the Royal College of Dental Surgeons of Ontario produced a guideline for the province's dentists and dental specialists. And, Ontario is expanding Rapid Access Clinics across the province to help people with hip, knee and lower back pain access the right treatment faster, including non-opioid treatments.
To provide a personal perspective of the issues raised by the data, the Health Quality Ontario report also features stories from patients and health care professionals.
Related findings:
- Canadians are the second-largest per-capita users of prescription opioids after the U.S. at over 34,000 daily doses per million in 2013-2015, according to the Report of the International Narcotics Control Board for 2016.
- About 44,000 health care professionals in Ontario prescribed opioids in 2016.
- Together, family doctors, surgeons, and dentists represented 86% of all new-start opioid prescriptions in 2016.
- In 2016, 865 people in Ontario died from opioid toxicity, up from 366 in 2003. Although many deaths involved opioids that were obtained from street sources, opioid-related deaths have also been shown to be concentrated among patients who are prescribed opioids more often, according to Public Health Ontario.
- Opioid related emergency department visits more than doubled to 4,427 in 2016 from 1,858 in 2003: Public Health Ontario.
To read the full report visit: www.hqontario.ca/StartingonOpioids
About Health Quality Ontario
Health Quality Ontario is the provincial advisor on the quality of health care. With the goal of excellent care for all Ontarians, Health Quality Ontario reports to the public on how the system is performing, develops standards for what quality care looks like, evaluates the effectiveness of health care technologies and services, and promotes quality improvement aimed at sustainable positive change. Visit www.hqontario.ca for more information.
SOURCE Health Quality Ontario

What are YogaPaws?
YogaPaws gloves and socks are made out of an ergonomic design that keeps the webbing of the hands and feet happy while you exercise. The thick pads encourage correct posture and technique while providing all the comfort and support that Yogi desires. Finger and toe cutouts allow you to take full control of your positioning, while fitted palm and feet coverage boosts your balance and helps evenly distribute your weight while in movement. The gear makes exercising both indoors and outdoors feel effortless and natural - just like it should.
Why YogaPaws?
YogaPaws allow you to practice yoga anytime, anywhere, without the use of a mat. They’re convenient to pack lightly, and have many different uses, too. Check out other ways yogis are using their gloves and socks here! Plus, it’s not just for women – there are men’s sizes and options available, too.
Where can YogaPaws be purchased?
Online, at several different retailers, including their website and Amazon, YogaOutlet.com and more.

Other info & Quick Stats
Click here for the company website: http://www.yogapaws.com
Interview: Jamie Getwiller, CEO/inventor
YogaPaws is a mother/daughter adventure which started in 2001 and officially in launched in 2003. Gail (mother) and Jamie (daughter) Getzwiller share a love for travel and yoga which lead to a natural development of the YogaPaws. Since then, they have embarked on a journey of love and working dedication to produce the best “paws” possible. Yoga Paws have been a product and company that cares about spreading the love and allowing all the yogi's around the world to enjoy as non-slip practice, anytime, anywhere.
Pricing: Full sets begin at $35.00 and in a variety of sizes, ranging from petite, wide and regular.
Donation and Transplant in Ontario Makes Headway in Last 10 Years
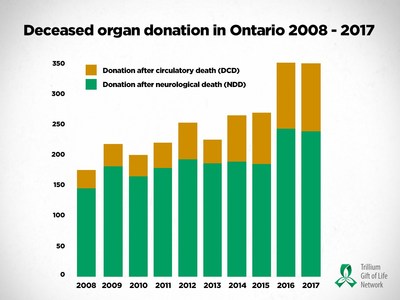
TORONTO, Jan. 24, 2018 /CNW/ - Since 2008, the number of deceased organ donors in Ontario has nearly doubled, increasing by 98 per cent.
Trillium Gift of Life Network (TGLN), Ontario's government agency responsible for organ and tissue donation and transplantation, released its 2017 results today and reviews its progress over the past 10 years (January 1, 2008 – December 31, 2017).
TGLN has applied a number of leading practices that have contributed to its success over the last decade, including: implementing routine notification at 69 hospital corporations, which requires hospitals to refer all potential donation cases to TGLN, and appointing 58 donation physicians that work alongside the hospitals' executive and operational staff and TGLN to ensure donation is part of quality end-of-life care.
Ontario is a leader in donation
In 2017, there were 347 deceased organ donors compared to 175 in 2008.
TGLN's leading practices have included the application of donation after circulatory death (DCD), which, in conjunction with other advanced efforts, has been a significant contributor to the growth of deceased organ donors in Ontario.
There are two types of donation after death: donation after neurological death (NDD) and donation after circulatory death (DCD). DCD is an option when a patient has a severe neurological injury, with no chance for recovery, and the decision to withdraw life-sustaining treatment has been made. The first DCD case in modern Canadian history was performed in Ontario in 2006. In the last 10 years, DCD has increased by 260 per cent and today, approximately 1 in 3 organ donors are a result of DCD.
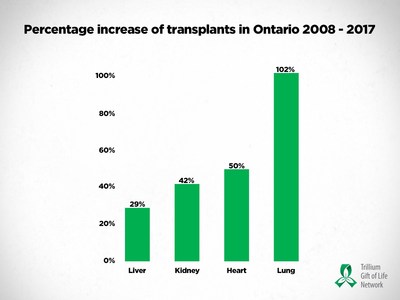
Similarly, as a result of the expansion of routine notification from 21 hospitals in 2011 to 69 hospital corporations today, the number of tissue donors has climbed considerably, growing 102 per cent from 1,061 in 2008 to 2,141 in 2017.
One tissue donor can enhance the lives of up to 75 people: eyes can restore sight; skin can help burn patients; bone can be used for joint replacements; heart valves can help patients with congenital heart disease; and tendons and ligaments can help people walk and run.
Transplant performance results give people hope
Largely due to the rise in deceased donation, the number of organ transplants in Ontario has increased by 46 per cent in the last 10 years (1,268 in 2017 compared to 867 in 2008). However, despite the increase in both donation and transplant, the need for transplant continues to outweigh the number of organs available for transplant.
"We all, as Ontarians, deserve to feel great pride in the advancements in our province's donation and transplant system," said Ronnie Gavsie, President and CEO, Trillium Gift of Life Network. "More and more medical conditions are being treated by organ transplant; more and more lives are being saved; we have an internationally renowned system. But as long as there are people waiting for a lifesaving organ transplant, there is much more to be done. Together, with our committed hospital partners, we are continuously working to make improvements to ensure that there are no missed opportunities for donation."
A culture of donation in Ontario
In 2008, only 16 per cent of eligible Ontarians were registered. Today, 32 per cent (nearly four million Ontarians) have registered their consent to organ and tissue donation. Over the last ten years, the number of registered organ and tissue donors have grown by 126 per cent.
"Ontario's success in organ donation and transplant is only possible because of the incredible donors and their families who make the generous and difficult decision to give the gift of life," said Dr. Eric Hoskins, Ontario's Minister of Health and Long Term Care. "Because of their gift, over 1,200 people were given a second chance at life in 2017. Register today at www.BeADonor.ca and give hope to the 1,500 people waiting."
Trillium Gift of Life Network is a not-for-profit agency of the Government of Ontario responsible for planning, promoting, coordinating and supporting organ and tissue donation for transplantation across Ontario and improving the system so that more lives can be saved.
SOURCE Trillium Gift of Life Network
Canadian patients to benefit from major investment in genomics and precision health research
Government of Canada and partners invest $255 million in genomics research bringing new hope for Canadians living with cancer, cystic fibrosis, juvenile arthritis, childhood asthma and other diseases.
TORONTO, Jan. 23, 2018 /CNW/ - Precision health promises to transform the way Canadians receive medical care. In the near future, doctors may be able to precisely diagnose symptoms based on a patient's unique genetic makeup and offer them tailor-made treatments that can save the patient's life.
To help make that possibility a reality, the Government of Canada announced two new major investments in genomics research totalling $255 million from federal and provincial governments, as well as research institutions and private sector partners.
The federal Minister of Science, the Honourable Kirsty Duncan, made the announcements at The Hospital for Sick Children (SickKids) in Toronto, where she highlighted a $162 million investment through Genome Canada, the Canadian Institutes of Health Research and co-funding partners, in 15 genomics and precision health projects across Canada.
The projects funded at SickKids will provide targeted treatments for children with brain cancer and will transform treatment for children living with arthritis. The funding also supports a targeted initiative to address health challenges facing Indigenous populations, improving diagnostic outcomes for Indigenous children that have genetic diseases.
Minister Duncan also announced a second major investment to support advanced genomics technology platforms across the country. These technology platforms support the development of improved technologies that underpin research advances in health, agriculture and natural resources. A total of $93 million is being invested in 10 platforms nationwide, with $45 million in federal funding through Genome Canada and an additional $48 million from other sources.
The combined totals of these two investments will provide researchers with access to cutting-edge tools, technologies and services while furthering the Government of Canada's goal to strengthen and support the country's scientific community.
Quotes
"It is an honour to support some of Canada's leading genomics and precision health researchers through investments that will allow them to further their discoveries and innovations. Their incredible work brings hope to Canadians living with chronic illnesses, such as cancer, cystic fibrosis and arthritis, while strengthening Canada's health-care system."
– Honourable Kirsty Duncan, Minister of Science
"All Canadians stand to benefit from the innovative and collaborative research projects being announced today. The platforms, tools, technologies and services that will be developed through this funding will improve our understanding of many illnesses, particularly those that affect the most vulnerable patients, including children and Indigenous peoples."
– Honourable Ginette Petitpas Taylor, Minister of Health
"What's exciting about these genomics and precision health projects is how clinically-oriented they are. Most are led by clinical scientists who deal with patients on a day-to-day basis and are well positioned to apply the research to health-care settings. Further, they are not just about developing new therapies to treat diseases, but about early diagnosis and intervention to better curb or manage diseases at their onset."
– Mr. Marc LePage, President and CEO, Genome Canada
"Our understanding of the human genome and epigenetics is advancing at an unprecedented pace. As a result, today we are creating knowledge that will improve health and health care delivery in ways that were unimaginable only years ago. CIHR is proud to partner with Genome Canada on this important initiative, and to support the outstanding scientists who are at the forefront of this rapidly growing field of research."
– Dr. Roderick R. McInnes, Acting President, Canadian Institutes of Health Research
Quick facts
Associated links
Backgrounder – precision health projects
Backgrounder – genomics technology platforms
This event will be livestreamed on Genome Canada's Facebook page. Also follow us on Twitter, LinkedIn and YouTube @GenomeCanada
Follow Minister Duncan on social media.
Twitter: @ScienceMin
Instagram: sciencemin
SOURCE Genome Canada
BEST HAIR TIPS FOR GIRLS WITH NATURAL CURLS
International Stylist and Curl Master Creator of The Doux
Gets Real About Real Hair

People with wavy or curly hair are always looking for new products, tips and tricks to lock in their desired look. Whether they want to blow it straight, create looser curls or maximize their tighter coils, Maya Smith, Celebrity Hair Stylist, salon owner and creator of The Doux, the “Indie” haircare line with cult following available at Target is truly the master. Here she shares her best tips for girls with curls who want to revel in their natural hair and create a style they love.
Understand the battle between oil and moisture.
The first thing people must understand is that there are opposite things going on at the same time. “Due to the shape of curly haired strands, the hair tends to be under moisturized. On the other hand, the curly haired scalp can get very oily. Managing these opposite demands is the struggle of girls who wish to keep their curls. The key here is knowing how best to address both,” explains Maya who led the movement for women to transition from relaxers to natural curls.
Be gentle when washing curly hair.
According to Maya, kinky, thick, coiled textures tend to appear “tough” and strong enough to withstand heavy manipulation. “In my experience, these hair types are actually the most delicate, and should be handled with care, she recommends.”
Step One: Pick your products wisely.
Maya applied over 2 decades of research and development based on working knowledge of hair texture and listening to what people wanted. “I created The Doux™ SUCKA FREE Moisturizing Shampoo and FRESH RINSE Moisturizing Conditioner as the one-two step that delivers both deep cleaning plus exceptional nourishment necessary for styling.” It’s now available in Target stores and the full product line is available online at www.thedoux.com.
Step Two: Prep for shampoo.
Maya’s professional instructions for curl mastery begins with rinsing hair thoroughly with water for a minimum of 30 seconds. “This helps to eliminate any water-soluble product buildup, such as hair gel or heat protectant. It also helps you save shampoo! Assuming you’re shampooing in the shower, letting the water run over the hair in a downward motion helps prevent further tangling, and allows the hair shaft to swell and the curl pattern to fully rebound.” For those with extremely thick hair, Maya suggests separating hair into 4 sections prior to wetting the hair for increased manageability.
Once the shampoo is applied, Maya recommends light manipulation at the scalp, going from the crown of the head to the nape of the neck. “Squishing” the hair up toward the scalp is a no-no. “Shampooing this way can cause unforgivable tangling and matting. I recommend repeating the shampooing process at least once.”
Step Three: Condition and comb through like a pro.
If your scalp was properly shampooed, conditioning is easy. “This time, you’re focusing on your thirsty ends first, working upward toward the scalp. Gently detangle with a wide-toothed comb or detangling brush (our favorite is Felicia Leatherwood’s “Brush with the Best” detangling brush) before rinsing, starting at the ends, working up toward to the roots. Remember to rinse with cool water which snaps cuticles shut, locks in moisture, makes your hair shinier and reduces frizz.”
When it comes to “co-washing” or “conditioner washing” Maya equates the popular trend to washing your clothes with fabric softener. “In my experience, co-washing causes build-up on the hair, coating the cuticle and impairing the hair’s natural ability to absorb water. Oils, waxes, and product residue harden on the hair shaft, making it more brittle and less porous over time. When the hair can no longer effectively absorb water, the elasticity of the hair is compromised, leaving the hair “crunchy” and stiff, where it is more likely to break. The result is hair that feels dry and brittle, no matter what product you use to moisturize it,” explains Maya.
One of the things Maya Smith and her team of stylists are known for is their ability to restore hundreds of their clients’ curls, simply by getting them to trade in the co-wash for a gentle, pH-balanced moisturizing shampoo, like The Doux’s SUCKA FREE which properly cleanses hair of product residue. “Once you have the hair thoroughly clean it “drinks” up the necessary amount of moisture, and returns to its natural softness,” Maya clarifies.
Avoid alcohol and kick the crunch to the curb.
Styling products high in alcohol give curls a crunchy feel. They suck up every last bit of moisture. Hair spray tends to contain the most alcohol, while gels, mousses and anything that provides hold or lift come in second. “I recommend water-soluble gels that don't feel sticky on your skin, and aerated mousses or foams that resemble beaten egg whites, to give hair fullness, control, and non-brittle curls,” Maya says.
She adds that she created The Doux so it can be used on hair that is worn curly or straight. “Our clients purchase one set of products, and apply them differently to achieve the style they want. If you’re rocking curly hair today, you’re using The Doux’s Mousse Def and Bonita Afro Balm for softness and definition, and The Light for shine. If you’re wearing a blowout, you’re still using the same products, but applying them less liberally, and using the shine mist as a heat protectant. It’s super simple and easy to follow once you’ve seen the results each of them deliver,” Maya explains.
Blow-Dry with a diffuser or hooded dryer.
Maya’s first choice for curly styles is to air dry. “If you don’t have the time to air dry then dry with a diffuser or hooded dryer on a low heat setting. A regular blow dryer nozzle disrupts the curl pattern and focuses hot air on one small section at a time while a diffuser, dries curls evenly for a full, uniform look,” she explains.
Maya recommends always applying a heat-protecting product, then flipping your head upside down using a diffuser at the roots and mid-length making sure to dry the area completely to lock in volume. “It’s important to leave the ends for last, and leave them only semi-dry. Air drying the ends is your best option.”
Care for the curls you were born with!
About Maya Smith:
Maya Smith is an International Master Stylist and Founder of The Doux Salon and haircare line now available in Target. With over two decades of styling experience Maya dedicated two decades to cracking the code on curl care, maintenance and expert styling. When it comes to caring for one’s natural hair and styling it, Maya is the best there is.
While still in high school, Maya got her hair cutting license and graduated from beauty school. Soon after graduating high school, Maya began following her passion and worked as an assistant for celebrity stylist Tracy Johnson. She learned from Johnson and progressed as a hair stylist for celebrities and entertainers. Years later the military wife would relocate to Germany, where Maya opened up her first salon The HoneyComb, a mecca for textured hair care for women from all over Europe, The UK, and as far as Africa. Maya's unique system of textured hair styling sparked the development of The DOUX® haircare products, first launched overseas, and distributed throughout Germany, France, Italy, and the Netherlands.
Currently, Maya leads a carefully selected team of stylists at The DOUX® Salon in Macon, Georgia and on Christmas Eve 2017, celebrated the arrival of The DOUX® in Target stores nationwide. Maya Smith, wife, mom of 5 and savvy business woman is an example not just for women of color but for all women who believe their gifts can impact the world, striving for entrepreneurial endeavors with grace, ease and hustle.
DR. ARTHUR AGATSTON AVAILABLE FOR INTERVIEWS
Creator of the Agatston Calcium Score and Founder of the Heart-Healthy
South Beach Diet
|
|
|
| You’ve likely heard about President Trump’s recent physical examination as well as Sanjay Gupta’s reference to Trump’s calcium score as it relates to heart disease.
But what exactly is the calcium score, also known as the Agatston calcium score? How was it developed and how is it used today?
The Agatston score was created in 1990 and named after Dr. Arthur Agatston, founder of the heart-healthy South Beach Diet, who continues to practice cardiology in Miami Beach, Florida. The work leading to the Agatston calcium score was done at Mount Sinai Medical Center in Miami Beach in the late 1980s.
In short, because of the increasingly widespread use of cardiac CT imaging, the Agatston calcium score has received great scientific and clinical interest as it was the first approach to quantifying coronary artery calcium. Knowing a patient’s coronary artery calcium score facilitates a more informed physician-patient discussion and the decision of whether or not to go on decades-long statin therapy, which helps reduce the risk of a heart attack and stroke. |
|
|
|
|
|
ARTHUR AGATSTON, M.D.
Biography
Arthur Agatston, M.D., is the Medical Director of Wellness and Prevention for Baptist Health South Florida. A pioneer in cardiac disease prevention, Dr. Agatston worked with Dr. Warren Janowitz to formulate the Agatston Score, a method of screening for coronary calcium as an indicator of atherosclerosis that is used at medical centers throughout the world and considered by most experts to be the best single predictor of a future heart attack. Dr. Agatston is a clinical professor of medicine at Florida International University Herbert Wertheim College of Medicine and an associate professor of medicine at the University of Miami Miller School of Medicine. His cardiology practice in Miami Beach is focused on preventing heart attacks in high-risk patients.
Known as the author of the internationally best-selling book, The South Beach Diet, his first nonacademic work, Dr. Agatston created his balanced approach to healthy eating to help his patients improve their blood chemistries and lose weight. Today, the South Beach Diet is the trusted choice of millions and there are more than 23 million copies of The South Beach Diet and its companion books in print worldwide. The lifestyle program has grown to include Web-based materials and a family of healthy and convenient foods, including delicious and nutritionally balanced bars and snacks, as well as a popular online program, SouthBeachDiet.com. Dr. Agatston’s most recent books, The South Beach Diet Gluten Solution and The South Beach Diet Gluten Solution Cookbook, were published in 2013.
Dr. Agatston has published more than 100 scientific articles and abstracts in medical journals and is a frequent lecturer across the U.S. and around the world on diet, cardiac imaging, and the prevention of heart disease. In recognition of his contributions to cardiac prevention, the Society of Cardiovascular Computed Tomography (SCCT) created the prestigious Arthur S. Agatston Cardiovascular Disease Prevention Award in 2011, which is given annually to pioneers in cardiac prevention. Among his many television appearances, Dr. Agatston was featured along with President Bill Clinton on Sanjay Gupta’s 2011 CNN special, “The Last Heart Attack.” |
|